Path Chapter 29: The Eye (pages 1346-1357) Age
advertisement

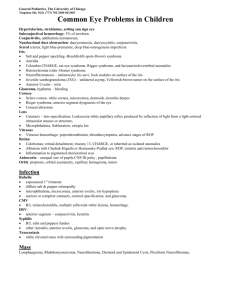
Path Chapter 29: The Eye (pages 1346-1357) Age-related macular degeneration (ARMD) is the most common cause of irreversible vision loss in the US The eye is a place where a doctor can easily visualize may different pathologies of the vascular system Page 1346 – anatomy of the eye Orbit – chamber that holds the eye, that is only open at its anterior So diseases that increase things in the orbit, displace the eye forward, called proptosis - - In proptosis, the eye might not get covered completely by the eyelids, or get enough tears across its cornea Cornea exposure is painful, and can predispose to corneal ulceration or infection In proptosis, where the thing that is enlarging is, will determine what direction the eye protrudes to o Things to the side of the eye, like the parotids, push they eye at an angle o Masses in the cone formed by the rectus muscles, like the optic nerve, push the straight out (axial proptosis) Axial proptosis is an important manifestion of grave’s disease at the thyroid o The proptosis is caused by accumulation of ECM proteins, & fibrosis in the rectus muscle The floor of the orbit is the roof of the maxillary sinus, and the medial wall of the orbit separates it from the ethmoidal sinuses - So uncontrolled sinus infection can spread to the orbit as an acute infection (orbital cellulitis) or from fungi (mucormycosis) in immunosuppressed people or diabetics Idiopathic orbital inflammation (orbital inflammatory pseudotumor) – can be inflammation of the whole orbit, or just localized in the lacrimal gland (sclerosing dacryoadenitis), extra-ocular muscles (orbital myositis), or Tenon’s capsule (fascia that wraps around the eye, causes posterior scleritis) - If you see vasculitis with necrotic collagen, it suggests Wegener granulomatosis Most primary tumors of the orbit are vascular - The most common primary tumors of the orbit are capillary hemangioma and lymphangiomas of infancy, and cavernous hemangiomas of adulthood The eyelid is made of skin externally, and then mucosa, called the conjunctiva, of the surface of the eye - The eyelid protects and covers the eye, and also has things to generate tears – page 1348 If the drainage system of the sebaceous glands is obstructed by chronic inflammation at the eyelid margin (called blepharitis), or by a tumor, lipids can leak into surrounding tissue and provoke a granulomatous response to form a chalazion (lipogranuloma) - - - Primary melonomas of the eyelid skin are rare The most common cancer of the eyelid is basal cell carcinoma Eyelid cancers can prevent the eyelids from closing completely, which hurts and predisposes them to corneal ulceration o Eyelid cancers don’t threaten their life, but you treat them quick to preserve vision Sebaceous carcinoma can look like eye inflammation or a chalazion, and spreads first to the parotid and submandibular nodes, with a higher mortality o Sebaceous carcinoma will show vacuolization of the cytoplasm to help diagnose In people with AIDs, Kaposi sarcoma can develop on the eyelid or conjunctiva o Kaposi sarcoma of the eyelid looks purple from blood vessels in the dermis, but in the conjunctiva it looks red The conjunctiva is divided into 3 zones: - - Palpebral conjunctiva – conjunctiva lining the interior of the eyelid o Palpebral conjunctiva is tethered to the tarsus Conjunctiva in the fornix – pseudostratified columnar epithelium rich in goblet cells (tears) o The fornix also has lacrimal tissue, and ductules from the main lacrimal gland o Most of the lymph cells in the conjunctiva are in the fornix These lymph follicles can enlarge enough in viral conjunctivitis to be seen by slit-lamp exam Granulomas from systemic sarcoidosis can be seen in the fornix Bulbar conjunctiva – conjunctiva that covers the surface of the eye o Bulbar conjunctiva is a nonkeratinizing stratified squamous epithelium Conjunctival scarring: - - When chlamydia trachomatis infects the conjunctiva (trachoma), it can cause conjunctival scarring A decrease in the # of goblet cells from conjunctival scarring decreases surface mucin, which is needed for adhering the aqueous part of tears to the corneal epithelium o So even if the aqueous part of the tear film is adequate, the person will have dry eye o Dry eye can hurt and predispose to corneal opacification and ulceration o Dry eye is more often caused though by a deficiency in the aqueous part of the tear film made by the lacrimal glands found in the eyelid and fornix Surgery to remove a conjunctival cancer or lesion can leave the person with dry eye from conjunctival scarring Pinguecula and pterygium are both submucosal elevations on the conjunctiva - They both result from actinic damage (sun), so they’re found in sun-exposed areas of the conjunctiva, mainly the opening between the upper and lower eyelids (intrapalpebral fissure) Pterygium usually originate in the conjunctiva next to the limbus o - Pterygium are formed by a submucosal growth of fibrovascular connective tissue that migrates on the cornea o Ptyergium don’t affect vision Pinguecula are small yellowing submucosal elevations next to (astride?) the limbus o Pinguecula don’t invade the cornea like the pterygium does, but it can cause uneven distribution of the tear film over the cornea The dehydration can cause a “saucer-like” depression in the corneal tissue, called a dellen Conjunctival tumors: - Both squamous and melanocytic cancers and their precursors, tend to develop at the limbus Conjunctival intraepithelial neoplasia (precursor to invasive squamous carcinoma) and squamous papillomas of the conjunctiva can both involve HPV’s 16 and 18 Pigmented lesions are most likely melanoma Nevi of the conjunctiva characteristically have subepithelial cysts lined by surface epithelium – page 1350 Conjunctival melanomas usually affect fair-skinned middle aged people – page 1350 o Conjunctival melanoma has a precursor lesion called primary acquired melanosis with atypia The sclera is made mainly of collagen, and has few blood vessels and fibroblasts - So wounds to the sclera heal poorly Immune complexes can deposit in the sclera in rheumoatoid arthritis, causing necrotizing scleritis “blue” sclera is seen in several problems: o The sclera can get thin after an episode of scleritis, making it’s normal brown color look blue o High intraocular pressure can also thin the sclera, making it look blue This lesion is called a staphyloma o The sclera can look blue in osteogenesis imperfecta (no collagen) o A very pigmented congenital nevus under the uvea, can make the sclera look blue, called congenital melanosis oculi When there’s also skin pigmentation around the eye, it’s called nevus of Ota The cornea and its overlying tear film, make up the major refractive surface of the eye (not the lens!) - Myopia (nearsighted) develops because the eye is too long for its refractive power Hyperopia (farsighted) results from an eye that is too short for its refractive power So cornea shape is very important in adding to the refractive power of the eye Anteriorly, the cornea is covered by epithelium sitting on a basement membrane called Descemet membrane o - - - - Underneath the basement membrane is the Bowman layer, which doesn’t have cells, and serves as a barrier against cancer from spreading from the epithelium to the underlying stroma The corneal stroma doesn’t have any blood vessels or lymphatics, which makes the cornea transparent, and also makes the cornea good at getting transplants Scarring and edema of the cornea both disrupt the alignment of the stroma collagen, adding to corenal opacification The corneal endothelium is derived from neural crest A decrease in endothelial cells or an endothelial problem in the cornea will cause stromal edema Descemet membrane gets thicker as you age, and is where the Kayser-Fleischer rings of Wilson’s disease are found Pathogens can cause corneal ulceration, leading to inflammation of the cornea, called keratitis o In keratitis, dissolution of the corneal stroma can be accelerated by activation of collagenases in the corneal epithelium and stromal fibroblasts (aka keratocytes) o When exudate and cells leak from the iris and ciliary body vessels into the anterior chamber, you can see it on slit-lamp exam, and it can accumulate into a hypopyon o Although corneal ulcers can be infectious, the hypopyon rarely contains organisms, showing how good the vascular response is here to acute inflammation Cornea problems are divided into corneal disorders and corneal dystrophies o Corneal degenerations can be either unilateral or bilateral, and are usually nonfamilial o Corneal dystrophies are usually bilateral, and hereditary Corneal degenerations: o Keratoconus – common disorder with progressive thinning and dilation of the cornea There is no inflammation or vascularization Keratoconus thinning happens in abnormal eyes that have conical-shaped corneas, instead of the normal spherical shape The abnormal shape causes an astigmatism that is hard to fix with glasses, but contacts can help If glasses or contacts don’t work, you do a corneal transplant Despite being a corneal degeneration, keratoconus is often bilateral Keratoconus happens often in Down syndrome and Marfan syndrome The hallmark of keratoconus is thinning of the cornea, with breaks in the Bowman layer Sometimes, the Descemet membrane can rupture, allowing aqueous humor from the anterior chamber, into the corneal stroma, called a corneal hydrops Corneal hydrops can cause sudden worsening of vision Corneal hydrops can lead to corneal scarring, which makes vision loss even worse Corneal dystrophies: o Band keratopathies: Calcific band keratopathy – calcium is deposited in the Bowman layer o o Often seen in chronic uveitis, especially with juvenile rheumatoid arthritis Actinic band keratopathy – happens from chronic exposure to lots of UV light from the sun The sunlight causes elastosis (accumulation of elastin) in the superficial corneal collagen of the sun-exposed interpalpabral fissure, causing horizontal bands The sun-damaged collagen looks yellow Fuchs endothelial dystrophy Fuchs endothelial dystrophy is one of the main indications for corneal transplants The 2 major manifestations of Fuchs endothelial dystrophy are edema and bullous keratopathy, which are both caused by loss of endothelial cells Early, the endothelial cells make “drop-like” deposits of abnormal basement membrane material (guttata) As it progresses, there’s a decrease in the # of endothelial cells, and the cells that are left can’t maintain stromal deturgescence (state of normal dehydration maintained by the cornea to keep it transparent) This causes the stroma to become edematous and thicken, giving it a groundglass appearance, and causing vision to blur If the # of endothelial cells decreases after cataract surgery, when they didn’t have previous Fuchs dystrophy, it’s called pseudophakic bullous keratopathy As stromal edema increases, the epithelium causes “hydropic change” and detaches the epithelium from the Bowman layer, causing a bullae that can rupture Fibrous connective tissue can be deposited between the epithelium and Bowman layer, called degenerative pannus Stromal dystrophies – the stroma deposits cause opacities in the cornea, which can decrease vision Macular corneal dystrophy – when macular deposits of keratin develop in the corneal stroma Mutations to the TGFB1 gene, which codes for ECM protein keratoepithelin, can cause deposition of different kinds of protein deposits in the cornea Lattice dystrophy – deposition of needle-shaped amyloid Granular dystrophy – deposition of chunky hyaline Anterior segment: - The borders of the anterior chamber: o Anterior – cornea o Lateral – trabecular meshwork o Posterior – iris - - - - Aqueous humor is formed by the pars plicata of the ciliary body o It then enters the posterior chamber, bathes the lens, and goes through the pupil to enter the anterior chamber The lens is a closed epithelial system, and its basement membrane (called the lens capsule) totally envelops the lens o So lens epithelium doesn’t exfoliate, like the skin epidermis would Instead, the lens epithelium and its fibers accumulate within the lens capsule, called “infoliating” So as you age, the size of the lens increases Cataract – lens opacity o Cataracts can be congenital or acquired o Things that can cause cataracts include galactosemia, diabetes, Wilson’s disease, corticosteroids, radiation, and trauma o Age can also cause cataracts, from nuclear sclerosis (opacification of the lens nucleus) o Urochrome pigment can accumulate and make the lens nucleus brown, making it so you can’t perceive blue color o To treat cataracts, you can remove the lens contents but leave the lens capsule intact, called extracapsular cataract extraction, or you can put in a prosthetic lens o Morgagnian cataract – when the lens cortex almost entirely liquefies This can cause high molecular weight proteins to leak through the lens capsule, called phacolysis, and then clog the trabecular meshwork, increasing intraocular pressure (glaucoma) and possible hurting the optic nerve Glaucoma - diseases characterized by changes in the visual field, and in the cup and optic nerve o Most glaucomas are associated with increased intra-ocular pressure o Aqueous humor is made in the ciliary body, and passes from the posterior chamber through the pupil into the anterior chamber – page 1354 To get there, most of the aqueous humor drains through the trabecular meshwork, found at the angle formed by the intersection between the cornea and the iris o 2 categories of glaucoma: Open-angle glaucoma – the aqueous humor has complete access to the trabecular meshwork, and the increase in intra-ocular pressure results from an increased resistance to aqueous outflow in the open angle Angle-closure glaucoma – the iris adheres to the trabecular meshwork and physically impedes the movement of aqueous humor from the eye o Both types of glaucoma can be primary or secondary o Primary open-angle glaucoma – most common form of glaucoma The angle is open, and few changes are seen Primary open-angle glaucoma can be caused by mutations to MYOC o Secondary open-angle glaucoma – when things clog the trabecular meshwork in the presence of an open angle - Elevations in pressure on the surface of the eye when there’s an open angle, can also cause open-angle glaucoma Happens in Sturge-Weber syndrome o Primary angle-closure glaucoma – usually develops in eyes with shallow anterior chambers, often in people with hyperopia (farsightedness) When the pupil margin of the iris connects to the anterior surface of the lens, it can obstruct flow of aqueous humor through the pupillary aperature, called a pupillary block Continued making of aqueous humor by the ciliary body then increases pressure in the posterior chamber, and can bow the iris periphery forward, connecting it to the trabecular meshwork, causing increased intra-ocular pressure You’ll see subcapsular opacities, called glaukomflecken o Secondary angle-closure glaucoma: Contraction of many kinds of pathologic membranes that formed over the surface of the iris, can draw the iris over the trabecular meshwork, occluding aqueous outflow Chronic retinal ischemia increases VEGF for angiogenesis, which forms a transparent membrane over the surface of the iris, which can contract to cause occlusion of the trabecular meshwork by the iris This is called neovascular glaucoma Tumors in the ciliary body can compress the iris onto the trabecular meshwork, closing off the major pathway of aqueous outflow In intra-ocular inflammation, vessels in the ciliary body and iris get leaky, allowing exudate to accumulate in the anterior chamber o The inflammatory cells can sometimes adhere to the corneal endothelium, forming keratic precipitates o Exudate can cause adhesions between the iris and the trabecular meshwork of the cornea, called an anterior synechiae, or between the iris and anterior surface of the lens, called a posterior synechiae Anterior synechiae can increase intra-ocular pressure Prolonged contact between the iris and lens can deprive the lens of aqueous humor, causing fibrous metaplasia of the lens epithelium ,called anterior subcapsular cataract You use drugs to induce pupil dilation in people with intra-ocular inflammation, in order to prevent formation of synechiae o Endophthalmitis – inflammation within the vitreous humor The vitreous humor is next to the retina, so endophthalmitis hurts the retina o Panophthalmitis – inflammation within the eye that involves the retina, choroid, and sclera, and extends into the orbit Uvea – the iris, choroid, and ciliary body - - The uvea is one of the most vascularized parts of the body, but has no lymphatics Uveitis – inflammation in any of the tissues that make up the uvea o Uveitis can involve either just the anterior segment, or both the anterior and posterior o Uveitis usually hurts the retina o Granulomatous uveitis is a common complication of sarcoidosis There’s an exudate in the anterior segment that evolves into “mutton-fat” keratic precipitates In the retina, there can be perivascular inflammation, showing characteristic “candle wax drippings” o Toxoplasmosis often causes uveitis o People with AIDS often get CMV caused retinitis and uveitis o Injured eyes can develop sympathetic opthalmia, which is a noninfectious endogenous cause of uveitis that is bilateral The injury exposed retinal antigens the body doesn’t normally see, which got into the lymph and caused a hypersensitivity rxn that involves both eyes Can develop weeks to years after the injury Shows diffuse granulomatous inflammation of the uvea, sometimes with eosinophils The most common eye malignancy of adults is metastasis to the uvea, usually the choroid o It is very fatal very quick Uveal melanoma is the most common primary intra-ocular malignancy in adults o The nevi is common (10% of people) but it’s more rare for it to progress to melanoma o Since there’s no lymph in the eye, uveal melonmas spread by the blood, first ot the liver o It has spindle and epitheliod cells The more epitheliod cells, the worse the prognosis o Uveal melonomas can cause retinal detachment or glaucoma, affecting vision