BUPHTHALMOS
advertisement
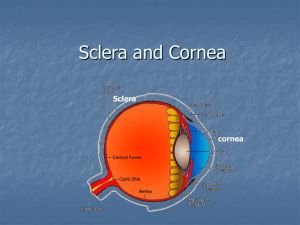
Increase in IOP restricted to developmental abnormalities in trabecular meshwork in the angle of the eye in absence of other secondary causes or related systemic congenital anomalies (e.g: Sturge-Weber syndrome, Neurofibromatosis, Lowe syndrome etc.) Only 1% from all glaucoma 75% Bilateral 65% Male 80% diagnoses in the first year of life Most cases appear to be sporadic However, an autosomal recessive pattern of transmission of the disease is evidenced In all developmental glaucoma, there is maldevelopment of iridocorneal angle (goniodysgenesis) which includes:1) Trabeculodysgenesis: maldevelopment of the trabecular meshwork 2) Corneodysgenesis: maldevelopment of the cornea 3) Iridodysgenesis: maldevelopment of the iris. The hallmark for developmental glaucoma is isolated trabeculodysgenesis. Normal trabecular meshwork Underdeveloped trabecular meshwork (Trabeculodysgenesis) Early: Triad of photophobia, epiphora and blepharospasm Due to corneal edema Late: Hazy cornea Large eye “ox eye” Defective vision Cornea Large & hazy Increased corneal diameter Normal = 10.5 mm Buphthalmos = > 12 mm Haab’s striae: transverse, tears in Descemet’s membrane Sclera Bluish discoloration due to thinning of sclera Anterior chamber Deep: due to bulging of cornea & flattening of lens Iris Iridodenesis (tremulous) May have stromal hypoplasia Pupil Sluggish reaction Lens Phacodenesis (tremulous) Relatively small and displaced posteriorly Flattened due to stretching of the suspensory ligaments Fundus Glaucomatous optic cupping (late) Refraction Axial myopia, but less than expected, due to:1) Flat cornea 2) Flat lens 3) Deep anterior chamber and the lens is relatively become more posterior in position Increased tear lake in the left eye Increased corneal diameter of the left eye in comparison with the right eye Hazy cornea Haab's striae as seen on retroillumination Haab’s striae Haab’s striae Dense opacification of cornea in advanced cases Stromal edema superiorly (arrow) Positive family history Corneal assessment Corneal diameter more than 12 mm Haab’s striae Hazy cornea Tonometry Perkins handheld or Tono Pen is preferable in children IOP more than 21 mmHg IOP measured under general anaesthesia is less than real IOP due to:1) Effect of general anaesthesia 2) Low scleral rigidity 3) Flat cornea Gonioscopy Abnormal angle structures or membrane Iris is directly inserted into trabecular meshwork (either flat insertion or concave insertion) Ophthalmoscopy Glaucomatous cupping Cup to disc ratio is more than 0.3 Tono Pen Examination of a 3 months infant with buphthalmos under general anesthesia using Schiotz tonometer. Perkins handheld tonometer Treatment of buphthalmos is only surgical : Goniotomy Trabeculotomy Trabeculectomy Drainage devices Indication : Clear cornea with diameter less than 13mm. How? Goniotomy knife introduced in the A.C under gonioscopic control to cut the abnormal mesodermal membrane at the angle in 2/5 of the circumference. Result Goniotomy can successfully treat congenital glaucoma 80% to 90% of the time in cases the symptoms start when the child is 1 month to 2 years old. Complication The greatest complication after goniotomy is a return of high pressure in the eyes. If the pressure in the eye increases, the procedure may need to be repeated. Goniotomy Indication Corneal diameter more than 13mm or less than 13mm with hazy cornea. How? Trabeculotomy is performed from the scleral side at the limbus under the conjunctival flap. A fine wire-like instrument (trabeculotome) is inserted into Schlemm’s canal from an external incision and the trabecular meshwork is torn by rotating the instrument into the anterior chamber. Result Trabeculotomy can successfully treat congenital glaucoma 80% to 90% of the time in cases the symptoms start at the age of one month to two years old. Trabeculotomy is not as successful in children whose glaucoma was present at birth or began late in childhood. Complication The most common problem after trabeculotomy is scarring of the new opening in the eye which prevents fluid from draining out of the eye. Other complications : 1. Blurring of vision 2. Bleeding in the eye 3. Sudden, permanent loss of central vision 4. Infection in the eye 5. Malignant glaucoma is rare Trabeculotome Trabeculotomy Indication After failure of trabeculotomy or in advanced cases with corneal diameter more than 13mm. How ? Trabeculectomy is a surgical procedure involves removal of part of the trabeculum in the eye to relieve pressure caused by glaucoma. Procedures of trabeculectomy Trabeculectomy such as Molteno- seton implant or Ahmad’s valve are indicated in difficult recurrent cases where conventional procedure above failed. Molteno implant