362 HTN - MaryNursing2011
advertisement

Hypertension & Orthostatic HTN
1 – What normally remains relatively constant as
blood shifts from one area of body to another?
a. What does it rely on for adaptation?
BP
2 – BP relies on- Circadian Rhythms & Short-Term
Regulation for adaptation: Describe the short-term
regulation mechanisms
a. Examples of short-term regulation
chemoreceptors (sensitive to change)
Neural mechanisms
- Baroreceptors: pressure-sensitive
- Chemoreceptors: sensitive to change O2,
CO2, H+
Humoral mechanisms
- RAAS
- Vasopressin (ADH)
a.
3 – Humoral Mechanisms:
a. Antidiuretic hormone (ADH) is secreted
from Pituitary gland affects: thirst &
kidney -reabsorbs water extracellular
volume to affect serum osmolality and
blood volume. What happens in this system
when blood volume is too low?
b.
Circadian Rhythms (highest in the a.m;
natural drop right when waking up)
Short-Term Regulation
a.
O2, CO2, H+
a.
Pituitary gland releases ADH for
reabsorption
b.
Kidneys release Renin angiotensin
{converting enzyme: becomes reactive}
angiotension II Adrenal CORTEX &
Arterioles affected:
- Aldosterone: reabsorption by kidney: Incr
BP and vascular volume
- Vasoconstriction of systemic arterioles:
Incr arterial BP
What happens with the RAAS with low blood
pressure?
Things to know:
Systole: ejection (LV to Aorta)
Diastole: relaxation
Pulse Pressure: systole – diastole (~40)
Mean arterial pressure (MAP): Diastole + 1/3 pulse pressure Good indication of perfusion
BP = CO x PVR
Incr BP: HR, contractility; Incr PVR: vasoconstriction, viscosity
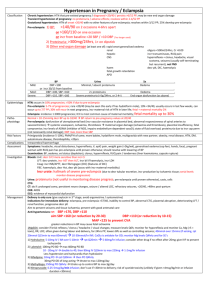
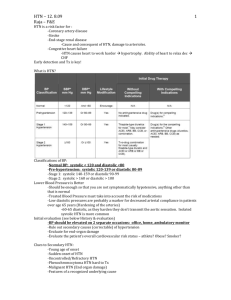
4 – This is consistent elevation of systemic arterial
BP
a. Also known as?
b. Causes?
Essential HTN
a. Idiopathic or primary
b. Unknown cause
95% of HTN cases
5 – This can be a diagnostic toola. BP= ?
b. CO= ?
c. What is under humoral control (SNS, local
vessel, RAAS)?
BP
6 – There are three types of HTN:
a. This is combined systolic & diastolic HTN
Essential, Secondary and Malignant
a. Essential (95% cases)
a.
b.
c.
CO x PVR
SV x HR
PVR
b.
This type of htn is altered hemodynamics
associated with primary disease (renal,
hormonal)
b.
Secondary (5-8% cases)
Malignant htn is progressive, diastole >120, causes
may be- encephalopathy, multi-organ damage leading
to death
7 – What causes HTN?
a. Factors relating to incr Co?
b. Factors relating to incr Total PVR?
Incr in CO and/or Total PVR
a. HR, SV
b. Viscosity, Vessel diameter
8 – Dx is based on?
MULTIPLE readings
Classification
Normal
Prehypertension
Stage 1 HTN
Stage 2 HTN
SBP
<120
120-139
140-159
>= 160
DBP
And <80
OR 80-89
OR 90-99
OR >= 100
Lifestyle Modifcation
Encouraged
Yes
Yes
Yes
***
9 – BP Classification:
a. Able to prevent
b. Give meds to prevent heart disease during
these stages
a.
b.
Prehypertension
Stage 1 and 2 HTN
Lifestyle modification is always done first
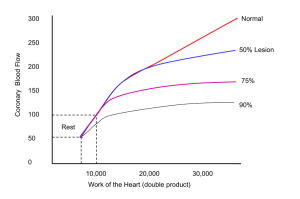
10 – Describe chronic damage in a blood vessel
lumen (which accelerates HTN)-
Prolong constriction & pressure thickening of
vessels impairs Prostacyclin (lipid molecule)
Arterial smooth muscle = hypertrophy & hyperplasia
Lumen (tunica intima, tunica media) narrow
permanently accelerates HTN
a.
b.
c.
What else is stimulated with injury of vessel
walls? Causing?
What happens as permeability incr?
Causing?
What are the effects of Ca as it enters the
vessel walls?
11 – Risk factors for HTN?
12 – HTN results from complicated interaction of
genetics and environment mediated by host of
a.
Biochemical mediators of inflammation
incr vascular endothelium permeability
b.
Proteins enter vessels (Na, Ca, Plasma
protein) further thickening
c.
Vasoconstriction (Smooth m. contraction
due to incr responsiveness to stimuli)
Family h/o
Aging
Race (African American)
Insulin resistance or metabolic disorders
Smoking
Obesity
Dietary sodium
Bcp
Stress
-
Incr blood vol.
Overactive RAAS
neurohumoral effects. What are some theories
associated with htn?
a. Interaction with many of these factors lead
to?
-
Na & H2o retention
Overactive SNS
Hormonal inhibition of Na/K pump
Interaction involving insulin resistance &
endothelial function (D.M.)
a.
Sustained Incr CO & PVR
13 – Renal hypertension (malignant),
pheochromocytoma, Cushing’s syndrome,
Coarctation of the aorta, Drugs (Pregnancy induced
after 20 wks gestation)- are primary disease which
may lead to which type of HTN?
Secondary HTN
14 – Pt’s with what primary diseases could lead them
to developing Secondary HTN?
Cushing’s
Pheochromocytoma
Renal HTN (malignant)
Drugs
Coarctation of aorta
Pregnancy induced
Complications
LV Hypertrophy –incr workload of left
ventricle (to compensate for incr pressure
leading to complications and end-organ
damage)
LVH HF
Renal failure (microalbuminuria)
Retinopathy (eye vessels)
IHD, CAD, Dysrhymmias
TIA, Stroke
Aneurysms
Artheriosclerosis, PAD
S&S
Early stage: (little)
- Incr BP
- Dizzy, headache
Years later:
- Damaged organs
“Silent Killer”
No symptoms until end stage
15 – What is one main complication due to HTN that
incr workload of LV?
Left Ventricular Hypertrophy (LVH)
16 – A pt with abnormal drop in BP (20 mmHg/10
mmHg), especially in the elderly- may have what?
a. Possible causes?
Orthostatic (postural) HTN
a. Acute: low blood vol.
drug-induce
immobility/bedrest
venous pooling
Chronic: disease (ANS)
also- vomiting, GI issues, fast elevators etc.
17 – With Orthostatic HTN, there is an absence of
normal circulatory reflexes or blood volume which
affects the body how?
Blood pools in lower extremities
So, when pt goes to stand: Decr CO BP falls and
a.
S&S?
there’s not enough blood going to the brain
a. Dizzy
blur vision
Syncope (black out)