Red Medicine MR
advertisement
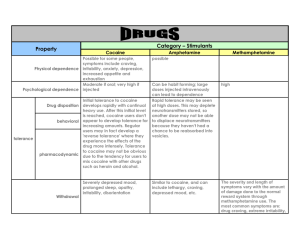
Red Medicine MR Nirav Pavasia Case C/C: My legs are in severe pain HPI: Pt is a 38 yo BM w/ PMH of HTN, cocaine abuser, presented to the ER w/ swelling and severe pain in both legs. Pt describes pain as sharp and burning, rates 10/10, tender to touch, nonradiating, associated w/ tightness, aggravated by movement and no relieving factors. Reports that the pain has been going on since 1 week but suddenly got worse last night and woke him up from sleep. Pt has not been able to ambulate 2/2 excruciating pain. Pt denies any similar episodes in the past. Pt has noticed subjective fevers and sweats for the past 2-3 days. Denies any trauma to the LE, recent travel, chest pain, SOB, n/v, dizziness, lightheadedness, abdominal pain, change in bowel or bladder habbits, wt loss or wt gain. ROS – Otherwise –ve unless stated per HPI PMH – HTN PSH – None FH – HTN, DMII, CAD SH – smokes 1.5 ppd, >20 yrs; drinks 12pk beer/day, >20 yrs; Snorts cocaine regularly – last use day before admission VS Temp: 38.3 Pulse: 104 BP: 169/95 RR: 18 O2 sat: 97% RA Allergies – NKDA Meds – HCTZ PE Gen – WN, WD, in mild distress due to severe LE pain LE – skin hot to touch, shiny, tightness and TTP in bilat LE, strength 3-4/5 due to pain, 4x5” palpable erythematic plaque like lesion in R calf, 2+ peripheral pulses bilat ext, no crepitus noted HEENT – NC/AT, EOMI, PERRLA, dry oral mucosa, no LADP, no JVD Chest – CTABL, no R/R/W CV – tachycardic, RRR, S1S2 nml, no M/R/G Abd – soft, NT, ND, NABS, no organomegaly Neurological – AAOx3, CN II-XII intact Labs WBC – 24.8 Na – 130 Hgb – 15 K – 4.4 Platelets – 198 Cl – 88 CO2 – 30 PT – 14.6 BUN – 19 INR – 1.2 Cr – 1.0 PTT – 24.8 Gluc – 106 Ca – 9.6 • CRP – 18 • ESR – 19 • Urine – Cocaine Pos Any thoughts? DDx Cellulitis DVT Superficial Thrombophelbitis Erysipelas Gas gangrene Necrotizing Fasciitis A/P Cellulitis – bilateral? Pt started on IV clindamycin, IV vancomycin blood cx Get US bilat LE to r/o DVT X-ray LE, CT LE w/ contrast to r/o gas gangrene and/or necrotizing fasciitis IVF Hospital course Pt continued to spike temperature for next 2 days, highest noted at 38.8 US LE: -ve for DVT X-ray, CT LE: wnl, no evidence of soft tissue edema, abscess, or gas noted. Normal limit LE w/o any pathology. No lymphedematous changes or any inflammatory changes were identified in either of the LE. The erythamatous plaque like lesion in the R calf now beginning to spread in centrifuge fashion towards proximally and appeared in LLE as well around the ankle and toes. Any thoughts? Ddx Henoch Schonlein Purpura (HSP) Hypersensitivity vasculitis Wegener Granulomatosis Churg-Strauss Syndrome (Allergic Granulomatosis) Polyarteritis nodosa Buerger Disease (Thromboangiitis Obliterans) Infective endocarditis Thrombotic Thrombocytopenic Purpura Cocaine induced pseudovasculitis Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis Further work-up ANA screen – negative w/ <1:40 CXR, ACE levels to r/o sarcoidosis – CXR unremarkable, ACE levels 59, CT chest – neg for hilar LADP or ILD HIV Ab – negative Hepatitis panel – non-reactive C3 – 151 C4 – 37 RPR – non-reactive TTE – negative for valvular lesions; normal EF; normal heart function CPK – high at 351 then trended down to 126 Hospital Course Pt was evaluated by dermatology service and Bx were taken Pathology report verbal read - neutrophilic infiltration around the small and medium size vessles showing leukocytoclastic vasculitis ANCA work up – negative Blood cx – negative Pt fever controlled w/ tylenol, continued to have severe 10/10 pain in LE, legs were less tight and shiny Hospital course Pt was started on solu-medrol 70mg IV per dermatology recs Over the course of 2-3 days pt’s pain much improved, rated 3-4/10 and erythamatous lesions began to fade away Vancomycin and Clindamycin stopped as WBC count normalized and pt afebrile for >3 days as well as clinical suspicion less likely for infectious etiology PT/OT consult placed – pt began to ambulate slowly Hospital course Rheumatology consult placed and… Rheumatology recs Cryoglobulin Human leukocyte elastase Lactoferrin Cathespin Lupus anticoagulant Beta-2 microglobulin 3-2 glycoprotein Hospital course Pt continued to improve Pain subsided to 1-2/10 and pt switched to PO steroids Pt was discharged home and was to follow up as outpt in 2 weeks with rheumatology clinic Ddx Cuatneous PAN (CPN) Hypersensitivity vasculitis Cocaine induced pseudovasculitis Thank you