Response to Draft Infant Feeding Guidelines
advertisement
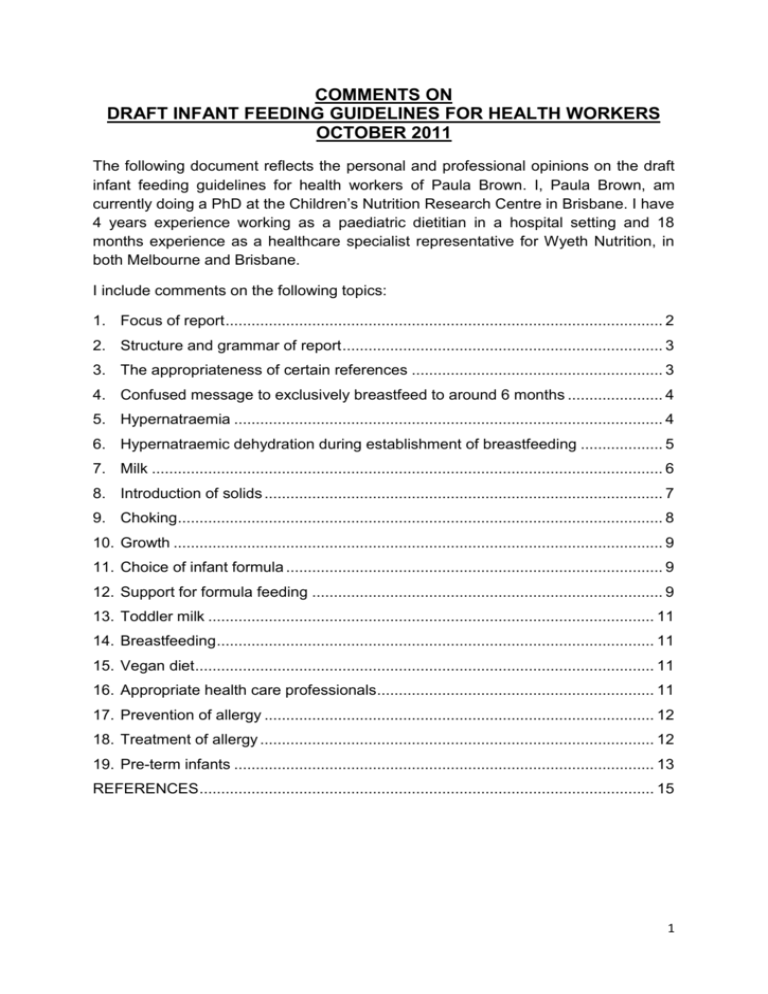
COMMENTS ON DRAFT INFANT FEEDING GUIDELINES FOR HEALTH WORKERS OCTOBER 2011 The following document reflects the personal and professional opinions on the draft infant feeding guidelines for health workers of Paula Brown. I, Paula Brown, am currently doing a PhD at the Children’s Nutrition Research Centre in Brisbane. I have 4 years experience working as a paediatric dietitian in a hospital setting and 18 months experience as a healthcare specialist representative for Wyeth Nutrition, in both Melbourne and Brisbane. I include comments on the following topics: 1. Focus of report ..................................................................................................... 2 2. Structure and grammar of report .......................................................................... 3 3. The appropriateness of certain references .......................................................... 3 4. Confused message to exclusively breastfeed to around 6 months ...................... 4 5. Hypernatraemia ................................................................................................... 4 6. Hypernatraemic dehydration during establishment of breastfeeding ................... 5 7. Milk ...................................................................................................................... 6 8. Introduction of solids ............................................................................................ 7 9. Choking................................................................................................................ 8 10. Growth ................................................................................................................. 9 11. Choice of infant formula ....................................................................................... 9 12. Support for formula feeding ................................................................................. 9 13. Toddler milk ....................................................................................................... 11 14. Breastfeeding ..................................................................................................... 11 15. Vegan diet .......................................................................................................... 11 16. Appropriate health care professionals................................................................ 11 17. Prevention of allergy .......................................................................................... 12 18. Treatment of allergy ........................................................................................... 12 19. Pre-term infants ................................................................................................. 13 REFERENCES ......................................................................................................... 15 1 1. Focus of report It is my opinion that this document is excessively long. The main focus of this document seems to be promoting breastfeeding rather than providing guidelines for infant feeding. 84 pages on the subject of breastfeeding is excessive, in a document of this sort. In contrast, only 13 pages are devoted to formula feeding and, 15 pages to the complex process of appropriate introduction of solids. Although I wholeheartedly agree that the promotion of breastfeeding is important for individual mothers and babies and the community, I suggest that this subject is given too much attention at the expense of other important issues. It may be the case that the excessive detail and discussion around the subject of breastfeeding could make this document confusing and inaccessible. The promotion of breastfeeding is a subject that is addressed and covered in a great number of easily accessible documents. Perhaps this document should focus simply on making practical recommendations regarding how breastfeeding should be encouraged and supported by healthcare professionals in Australia. Those interested in further detail or a full discussion of the evidence should be directed to the attached literature review or other relevant documents. Formula feeding and the introduction of solids are important issues, which are rarely addressed in other forums, and it is a great shame to see this opportunity to provide some much needed guidance on these issues being missed. In particular, 11 pages devoted to discussing the benefits of breastfeeding seems excessive. Perhaps this topic could be summarized into around 3 pages without the main points being lost. Discussion of the evidence surrounding this summary could be placed in the literature review. Areas which we feel could be removed entirely include page 37 where “Non-specific and pattern-specific protective factors in Breastmilk (Hale and Hartmann 2007)” are discussed in depth. This section: does not seem to add anything to the document; seems out of place; and is actually quite confusing and difficult to make sense of without additional reading. The discussion of the contraceptive effect of breastfeeding is of questionable relevance in a developed country. If “breastfeeding is not regarded as a reliable method of contraception for individual women in Australia”, women who do not want to become pregnant, should be using an alternative method of contraception. In a country where contraception is widely used and birth rates are low, there is little relevance to any benefit that may otherwise be seen on a “population wide basis”. The inclusion of this subject is more likely to result in some women being given a false sense of being protected from an unwanted pregnancy when breastfeeding, than to bring any benefit to the community. I also question the relevance of including a table with the nutritional composition of milk from different animals on page 57. 2 2. Structure and grammar of report There are certain areas where the structure does not seem logical to me. For example section 4.1 Hygiene on page 72, which is contained under “4. Breastfeeding: Common problems and their management”. I suggest this should be listed under “Section 2 Initiating, establishing and maintaining breastfeeding”. My impression of the quality of the writing is that it is not of standard that would be expected in such a document. Shorter sentences and the more liberal use of commas, would make the document easier to read and understand. For example on page 33 the sentence “There is probable evidence that infants from developing and developed countries who are exclusively breastfed for six months do not have deficits in growth compared to those who are not exclusively breastfed” would be easier to understand if commas where places as follows: There is probable evidence that infants, from developing and developed countries, who are exclusively breastfed for six months, do not have deficits in growth compared to those who are not exclusively breastfed. The following statements do not say what they intend to or do not make sense: Page 38: For infants with a strong history of atopy, standard infant formula are recommended, on medical advice. Page 56: Precipitation of the casein curd from milk produces whey that contains soluble proteins, lactose and many water-soluble minor components. Not only does this statement not make sense, it also appears to be factually wrong and irrelevant. Page 98: freshly expressed milk can be chilled in the refrigerator and added to frozen milk in the freezer. This does not make sense. Freshly expressed milk must be chilled in the refrigerator before being added to chilled or frozen breast milk, would make more sense. 3. The appropriateness of certain references I would like to question the following statement and reference on page 41 “The interdependence between the breastfeeding mother and infant, the regular close interaction and the skin-to-skin contact during breastfeeds encourage mutual responsiveness and attachment (Moore, Anderson et al. 2009).” This Cochrane review has the aim of investigating the impact of early skin to skin contact on various outcomes such as breastfeeding outcomes and maternal attachment behaviours. This reference provides no direct evidence that breastfeeding leads to improved attachment, as suggested by the statement. It could also be argued that the use of the word interdependence is inappropriate, seen as the mother is not dependant on the infant. On page 122 it is stated “The technique used by an infant to suck on the teat of a bottle differs from that used on the breast, and a use of a feeding cup instead of a bottle reduces the risk of nipple confusion (Righard and Alade, 1992)”. This reference describes a study where initial attachment success was correlated to 3 breastfeeding problems. The use of a feeding cup instead of a bottle was not investigated. I question whether there is any good quality evidence that nipple confusion is a true risk, which warrants discussion. 4. Confused message to exclusively breastfeed to around 6 months I have serious concerns with the inconsistent way that the message to exclusively breastfeed to around 6 months is communicated. On Page 3 this is defined in week as 22 to 26 weeks, which is actually 5 to 6 months. The message to exclusively breastfeed, to around 6 months, is repeated constantly throughout the document but rarely is the 22 to 26 weeks added e.g. on page 5. On page 42 it is stated: “Delay in the introduction of solid foods until after the age of six months is associated with increased risk of developing allergic syndromes”. This suggests that solids should be introduced before 6 months, whereas the guidelines to exclusively breastfeed until around 6 months, suggests that 6 months would be the ideal time to start weaning. This is confusing. It is also stated on page 42: “• Around six months is compatible with the “window of tolerance” postulated for the introduction of complementary foods to minimize allergies. • Around six months is defined as within four weeks of six months, ie 22-26 weeks” The use of ‘within four week of six months’ actually means 5 to 7 months. 22 to 26 weeks is 5 to 6 months, so around 6 months is actually being defined as up to 4 weeks before 6 months. There is no guidance on when, in this 4 week window, individual babies should begin having solids introduced. On page 8 it is stated “At around the age of six months (22 to 26 weeks), infants are physiologically and developmentally ready for new foods, textures and modes of feeding.” There is no reference to signs that may indicate a child is developmentally ready to wean. Would we suggest that all children should say their first word or take their first step at a particular age? I suggest that the guidelines should read to exclusively breastfeed until 4 to 6 months. To start introducing appropriate complementary foods, when your child is showing signs, that they are developmentally ready. This should be after 17 weeks but no later than 26 weeks. Signs that a child is developmentally ready shows be discussed in depth. 5. Hypernatraemia On page 8 it is stated “Do not add salt to food for infants”. The only mention of salt in the main body is on page 130: “Salty foods or very sweet foods should be avoided as these are acquired tastes that may result in poor foods choices later in life (Mennella and Beauchamp 1998).” This suggests that salt should not be added to an infant’s food solely for long term health promotion. The danger of hypernatraemia, associated with salt intake in infants, is not discussed. I suggest that on page 8 it is stated: A high salt intake is dangerous in infancy because infants have immature kidneys, so are unable to clear salt from their systems. Food high in salt should be 4 avoided and salt should not be added to food for infants. In section 10 Foods not suitable for infants or that should be used with care, salt should be mentioned first and the dangers should be discussed in detail. 6. Hypernatraemic dehydration during establishment of breastfeeding Under the heading of the sleepy newborn infant on page 64 it is stated “It is important that any medical causes are excluded before the infant is regarded as a ‘sleepy baby’. This will be apparent after several days. If all other causes are excluded – particularly incorrect attaching to and sucking at the breast – the mother must make sure she feeds the infant at least six times every 24 hours”. Under the heading of informed use of supplementary feeds in hospital on page 113 it is stated “If an infant has become dehydrated, rehydration may enable him or her to begin breastfeeding successfully. The infant’s condition should be discussed with the mother, and a paediatric assessment should be made before seeking the mother’s consent for rehydration. It should be emphasised, however, that such a situation is uncommon, even in the Australian climate. The implications of supplementary feeding for establishing and maintaining successful breastfeeding should be the subject of discussion between health worker and mother.” Under the heading Monitoring an infant’s progress on page 68 it is stated “The adequacy of breastfeeding can be assessed by observing the infant’s behaviour, feeding patterns, urine output and bowel actions, and by checking the infant’s weight and using growth reference charts.” These are all very important points and require much more discussion and prominence. These points must be made under one heading and the implications and dangers should be made explicit. The first few weeks of breastfeeding are a dangerous time. The insufficient intake of breast milk due to unsuccessful initiation of breastfeeding, can result in hypernatraemic dehydration, which can result in serious long term health consequences or even death. The incidence of hypernatraemic dehydration in breastfeed infants was found to be 4.1% in a Turkish study [1], 1.9% in a US study [2] and around 1.5% in a Swisse study. [3]. The incidence in Australia has not been studied, so it could be argued that stating it is uncommon, is not justified. It is quite possible that many mothers are dealing with this issue in the community by giving up on breastfeeding and starting formula feeds. With many mothers being discharged from maternity wards before lactation has been established it is vitally important that health care professionals are made aware of the risks. It should be recommended that every baby be closely monitored in the first few weeks of life to ensure that they do not lose more than 10% of their birth weight, they have regained their birth weight within 7 to 10 days and to ensure that breastfeeding has been successfully initiated. If hypernatraemic dehydration, is suspected the infant should be admitted to hospital and this issue should not be 5 managed in the community. In the interest of establishing exclusive breastfeeding successfully, I would like to see it recommended that infants are rehydrated using IV fluids and not dextrose solutions or infant formula. Mothers should be given rest, support and encouragement to allow the successful establishment of breastfeeding, should the mother wish to. 7. Milk On page 136 only 1 paragraph discusses the recommendation that infants below 12 months should not be given unmodified cow’s milk, and the reason given is due to a link with anaemia. On page 137 1 whole page is devoted to the dangers of consuming unmodified goats milk. I would like to point out that cow’s milk contains a similar protein content and renal solute load as goat’s milk. The risk of drinking unmodified cow’s milk are as great as drinking unmodified goat’s milk, and it could be argued that the uninformed early introduction of cow’s milk is a much larger issue than the misinformed used of unmodified goat’s milk. The early introduction of cow’s milk (before 12 months) is associated with increased renal solute load; increased blood loss from the gastrointestinal tract, contributing to iron deficiency and anaemia; chronic constipation and anal fissures; and an increased risk for subsequent type 1 and type 2 diabetes [4]. Prior to the regulation of the renal solute load of infant formulas in the UK in 1975 reports of hypernatraemic dehydration associated with the use of unmodified cow’s milk based formula where common [5, 6]. I would like to see an informed discussion informing all health care professionals on the risks associated with, infants below 12 months consuming any unmodified animal milks and are advised to ensure that all mothers are informed of this risk early in their child’s life to prevent the early introduction of these milks. When milk is discussed there seems to be some inconsistency and confusion. On page 7/8 it is stated: “It is not appropriate to use nutritionally incomplete alternate milks as the sole source of nutrition for infants. Pasteurised full cream cow’s milk is, however, an important component of a mixed diet for a child older than about 12 months. RECOMMENDATIONS Pasteurised full cream milk may be introduced to a child’s diet as a drink at around 12 months of age and be continued throughout the second year of life, and beyond. It is an excellent source of protein, calcium and other nutrients. Do not use unpasteurised cow’s or goat’s milk.” It is confusing that in places, pasteurised full cream cow’s milk is referred to and in other pasteurised full cream milk. The use of cow’s milk is a cultural influence and has no nutritional advantage over pasteurised full cream milks, from other animals. The position on goat’s milk products are unfounded and inconsistent. On page 123 it is stated that “the use of goat’s milk formula is not recommended”. While on page 137/8 it is stated “Goat’s milk-based infant formula is available in Australia and meets the standard for infant formula. A randomised controlled trial has shown no 6 differences in growth between cow’s milk and goat milk based formula (Grant, Rotherham et al. 2005). It has no advantages over cow’s milk based formula for the prevention of allergies and since there may be cross reactions with cow’s milk and goat’s milk protein, goat’s milk-based formula should not be recommended for infant’s with cow’s milk allergy (Grant, Rotherham et al. 2005)” .We suggest the statement on page 123 should read: there is no evidence of advantage of using a goat’s milk formula over a cow’s milk formula. 8. Introduction of solids The first 5 pages of this section are used to justify the guidelines to exclusively breastfeed until 6 months with regards to the adequacy of breast milk and allergy prevention. Only 4 pages are devoted to practical aspects of the introduction of solids and 5 pages to foods which should be avoided. The appropriate and safe introduction of solids is a complex process and there is a need for much more detailed information on this subject. On page 130 it is stated “The foods that are introduced should be of high nutrient density and include a variety of foods from all of the five food groups (Dewey 2005).” This is an important point and needs a lot more detail. The subject of texture is important and should have it own heading. The statement on page 130 “Increasing and varying food texture is essential for oral motor development. Infants not introduced to ‘lumpy’ textured food until after 10 months of age had greater feeding difficulties at 15 months than those introduced to lumpy food before six months, or between six and nine months of age” is important and should be given more prominence. I suggest that a recommendation be made and placed in the summary as follows; Infants should be offered food at an appropriate texture and consistency for their developmental stage. Increasing and varying food texture is essential for oral motor development. Lumpy textured food should be introduced between six and nine months. On page 132: Table IX.1 Developmental stages and examples of foods should really be replaced with something more appropriate. It is ineffectively summarising some very important points, that should be discussed more fully. There are also inaccuracies. For example toast fingers and rusks are given, as examples, of a pureed food. The around 6 months stage is defined as 21 to 30 weeks in this table, which is not consistent with the recommendation to start weaning at a minimum on 22 weeks. Rather than correct this in a note below, why not develop a relevant table. There are a number of food examples for the around 6 month stage and the 8 to 12 month stage and only pasteurised plain milk is given as an example of a family food after 12 months. It would be more useful if developmental stages and signs are discussed as one issue and examples of foods are dealt with separately. It would be useful to have examples for each food group for each texture and developmental stage. A list of suitable finger foods would be useful. Overall there are many important aspects regarding the introduction of solids which are not touched on: It would be nice to see much more discussion around the introduction of solids. Subjects that could be included include: 7 Developmental readiness for weaning e.g. loss of tongue thrust. Seating position of infant and feeder while feeding. The process of gradually increasing eating occasions with the aim of offering meals and snacks at regular and predictable intervals. The importance of offering small and regular meals due to small stomach size and high requirements A rough guide to normal portion sizes at 1 year of age. The social aspects of feeding. For example try to eat together as a family. Avoid distractions when feeding. The importance of feeding being a communication where the child cues are responded to e.g. offer appropriate amount of food and allow child to decide how much they eat. Learning self feeding. When cup feeding should begin and bottle feeding should be ceased. It would be nice for some discussion and a position statement on baby lead weaning. I refer you to the following references [7-9]. 9. Choking On page 8 it is stated: “Ensure spoon foods are of acceptable texture (no nuts or similar hard foods) and taste.” The example of nuts seems to be confusing the issue of choking with that of the progression from smooth purees to adult consistency food. On page 9 it is stated “hard, small and round, smooth and sticky solid foods are not recommended because they can cause choking and aspiration”. I question how these foods would cause aspiration. In this section food microbial safety and safe eating practices are both discussed under the heading of “caring for infants food”. These are unrelated and both important issues. I suggest that they be discussed separately. On page 64 it is recommended as a strategy “to rouse sleepy infants and encourage them to breastfeed”: “If the infant does not take the breast in spite of all efforts and is otherwise well, it is essential to express the colostrums and feed it by teaspoon, syringe or cup”. This strategy would appear to have a high risk of aspiration and choking. If it is to be suggested, perhaps it should be noted that this should only be done under careful supervision of a health care professional. The subject of choking is important from a safety perspective and also because the fear of choking is often a reason that infants are not offered increasingly textured foods. I would like the issue of choking to be discussed further with more discussion about risky foods and feeding practices e.g. forcing a child to eat. It may be worth considering that some infants will cough and splutter while learning to eat and parents should be counselled to expect this and how to deal with it, to prevent excessive anxiety which would interrupt the process of introducing increasingly textured foods. 8 10. Growth The second paragraph on page 125 discusses the importance of appropriate growth for long term health. This is an important point and should be discussed under its own heading. It would be nice to see a section devoted to healthy growth and growth monitoring. I would envision that this section would contain the following topics: The importance of “appropriate growth” What is appropriate growth in the context of breastfeeding, formula feeding and introduction of solids. The use of growth charts. The use of growth charts is currently discussed in appendix A. This is an important issue and would be better place within the main report, under this section. Guidance of the frequency and timing of weight, length and head circumference measurement. What action should be taken if growth is assessed, as excessive or inadequate. This could include advice for the breastfeed and formula fed baby separately. When a child should be referred to a paediatrician and/ or dietitian for further assessment. 11. Choice of infant formula On page 114 it is stated “interchange between formulas within the same generic group is optional and can be decided on the basis of cost”. This seems to suggest that parents choose the cheapest formula, which is typically a casein dominant formula, which would be closer in protein composition to cow’s milk than breast milk and are reported to be less well tolerated by infants . Is it being suggested that mothers should repeatedly change brands of formula depending which is on ‘special’? There is evidence to suggest that repeatedly switching between formula’s with different composition may lead to more gastrointestinal symptoms of feed intolerance in infants [10]. On page 116 it is stated “The reports of incorrect preparation of formula highlight the difficulties mothers face with differing scoop and instructions for different brands of formula”. I suggest that regular interchange between brands of formula is only likely to increase to risk of incorrect preparation of formula. I would also like to take this opportunity to request that to prevent confusion formula manufacturers are encouraged to standardise their scoop to water ratio, so that generic formula mixing instruction may be given. In the UK all infants formulas on the market are made with 30mls of water per 1 scoop of formula. 12. Support for formula feeding There is a danger that the vigorous promotion of breastfeeding has a negative impact on mothers who formula feed and their babies. There is evidence to suggest that formula feeding is associated with negative maternal emotions, such as guilt and 9 anxiety [11-13] and that mothers who formula feed are not given sufficient advice to ensure safe and appropriate feeding [11, 13]. The promotion of breastfeeding has often been focused on the initiation of breastfeeding, with midwifes and Baby Friendly Hospital Initiatives, receiving much attention and funding. There is a lack of easily accessible support in community, which means that many mothers are not provided with the support to overcome breastfeeding issues, and as a result end up formula feeding their infants. Other mothers may make an informed decision to formula feed, and once it has been confirmed that a mother has been suitably informed, this decision should be respected. Although it is important that all mothers be given information on the evidence based benefits of breastfeeding and be encouraged and supported to breastfeed for as long as they want to, it is also important that this is done in a manner which does not judge or exclude those who do not breastfeed. There is a real risk that mother who plan on formula feeding, will not disclose this fact to staff that are seen as being unsupportive of this decision, and will therefore not receive the information required to ensure the safe and appropriate use of formula. The recent use of the catchphrase “everyone looks up to mums who breastfed” is not evidence based and implies that people look down on those that do not, which is not helpful. Statements like “Any problem can be overcome” and a political commitment to providing services, which may provide mothers with the support to overcome these problems are more helpful. On page 116 it stated “The primary objective of the Code is to ensure safe and adequate nutrition for all infants. Health workers have a responsibility to promote breastfeeding first, but where needed, to educate parents on formula feeding”. This statement is not very conducive to formula feeding families being well supported. It would be more helpful to have a discussion where supporting formula feeding families is fully discussed with the following subjects being covered: How to promote breastfeeding when a mother expresses the wish to formula fed, in a manner which will not judge or exclude these mothers. That once it has been confirmed that a mother has made an informed choice to formula feed or that formula feeding would be the best option in the circumstances, that this decision should be respected and not repeatedly questioned. A detailed list of what education on formula feeding should be provided, by whom and when, should be included. This should include: a demonstration on the appropriate mixing of the formula that they plan to use at home, a discussion of the dangers of incorrectly mixed formula and sterilisation methods. This should be done on a one to one basis and parents should be provided with good quality written information. If parents do not understand English an interpreter should be used. Parents should be provided with details of where they can obtain support with formula feeding, once they go home. 10 All health care professionals involved in the care of infants should remain up to date and aware of issues surrounding formula feeding. 13. Toddler milk On page 115 it stated “Toddler’s formula milks are not necessary”. There is evidence that the use of iron fortified toddler milks, are an effective way of preventing anaemia, which is prevalent in this age group [14, 15]. 14. Breastfeeding On page 82 it is stated “Allow the infant to finish the first breast before offering the second breast. Always feed from each breast more than once each feed”. Perhaps this could be re-worded to be slightly more practical, for example: if the infant is still hungry after emptying both breasts, attempt to feed from each breast once more, before resorting to “top up bottle feeds”. In terms of expressing breast milk it would be good to see this discussed more fully, with techniques such as simultaneous pumping being recommended. I refer you to the Cochrane review on this subject [16]. 15. Vegan diet On page 12 it is stated “For vegan infants who are not breastfed or are partially breastfed, use of commercial soy based infant formula during the first two years of life is recommended. Dietetic advice may be necessary.” Soy based infant formulas are not vegan, because the vitamin D is grown on animal wool. I suggest it should be stated that there are no commercially available vegan formulas. A vegan family should be informed of this before discontinuing breastfeeding. If a vegan family choose to use a soy milk to feed their infant, they should be strongly recommended to use a soy based infant formula. Adult soy milks are equivalent to semi-skimmed milk, in terms of energy content, so would not be sufficiently energy dense for a child, below 2 years of age. 16. Appropriate health care professionals It is suggested that infants following a vegan diet may need the advice of a dietitian or appropriate health care professional and may require nutritional supplements. I suggest that an infant following a vegan diet will need the advice of a dietitian and will need a vitamin B12 supplement. I do not feel there are any other professions, that would be suitably informed and qualified, to give appropriate dietary advice in this circumstance. The same is true for the statement on page 10 “If food choices have to be restricted for medical reasons, the advice of a dietitian or appropriate health care professional should be sought to ensure that the dietary intake meets nutrient and energy needs”. 11 17. Prevention of allergy The prevention of allergy is discussed on page 40 in relation to breastfeeding and on page 122 in relation to soy formula and again on page 128 with relation to the introduction of solids. This is confusing. It may be more useful to have a separate section in which the prevention and treatment of allergy are discussed. I am pleased to see that the use of partially hydrolysed formula for allergy prevention is not recommended, as there is very little evidence for this. I suggest that partially hydrolysed formulas are specifically mentioned, in the same way that soy and goat’s milk based formulas, as not being recommended for the prevention of allergy. I would also like the appropriateness of the widespread use of partially hydrolysed formula for healthy infants, to be questioned. There is evidence to suggest that formula based on protein hydrolysate, are not nutritionally equivalent to formula based on whole protein [17, 18]. I especially have concerns about the use of partially hydrolysed formula in preterm infants, as evidence suggests there is no advantage and the use of these formulas is associated with a statistically significant reduction in plasma calcium and phosphate levels, despite a 9.6% higher intake of phosphate in the group fed partially hydrolysed formula [19].I am concerned that the impact of the disruption of intrinsic protein structure on issues such as calcium and phosphate utilisation and bone mineralisation, has not been fully explored in term and preterm infants. I would also like it to be noted that often hydrolysed products use pork enzymes to hydrolyse the product, so will not be appropriate for certain cultural groups. 18. Treatment of allergy On page 91 it is stated “If formula fed, these infants may benefit from switching from a standard to a hydrolysed formula. Anecdotal evidence suggests that a fully breastfed infant with GOR and such features may benefit from maternal dietary elimination of suspected proteins (Vandenplas, Rudolph et al. 2009), ”. Vandenplas et al [20] states “A subset of infants with allergy to cow’s milk protein experience regurgitation and vomiting indistinguishable from that associated with physiologic GER. In these infants, vomiting frequency decreases significantly (usually within 2 weeks) after the elimination of cow’s milk protein from the diet, and reintroduction causes recurrence of symptoms Studies support the use of extensively hydrolysed or amino acid formula in formula-fed infants with bothersome regurgitation and vomiting for trials lasting up to 4 weeks (206–208). Cow’s milk protein and other proteins pass into human breast milk in small quantities. Breast-fed infants with regurgitation and vomiting may therefore benefit from a trial of withdrawal of cow’s milk and eggs from the maternal diet (209,210). The symptoms of infant reflux are almost never so severe that breast-feeding should be discontinued” and recommendes “Management may include a 2-week trial of 12 extensively hydrolyzed formula or amino acid–based formula to exclude cow’s milk allergy, increased caloric density of formula and/or thickened formula, and education as to appropriate daily formula volume required for normal growth.” It is important that you refer to extensively hydrolysed formula or amino acid-based formula and not just hydrolysed formula, which could be considered to include partially hydrolysed formula, which would not be appropriate. It is also important that a 2 week trial of allergen avoidance be recommended and not simply a switching of formula or maternal dietary elimination, which implies a permanent change, even if no benefit is experienced. If a child is having solid food and/or some breastmilk a trial of extensively hydrolysed or amino acid based formula, without complete exclusion of allergens from the infant and mother’s diet will be ineffective. What is being recommended here is complex and has severe implications, so it should be explicitly stated that this should be undertaken under the supervision of a paediatrician and dietitian only. In terms of treatment of diagnosed allergy I would like to see it stated that an infant with a diagnosed allergy can continue to be exclusively breastfed, but the mother may need to exclude the allergen from her diet. This should be done with paediatric and dietetic supervision. It should be noted that partially hydrolysed formula and goat’s formula are not appropriate for the treatment of cow’s milk protein intolerance and that many children who are intolerant to cow’s milk will also be intolerant of soy protein. In my experience many health care professionals who advise parents on feeding are quite confused by lactose intolerance and cow’s milk protein intolerance. Could I suggest that a paragraph be devoted to this subject and it be made clear that while an extensively hydrolysed, elemental or soy formula can be used in both situations a lactose free formula should be used only for lactose intolerance. It may be worth discussing the fact that breast milk contains lactose but also lactase. In some cases breastfeeding may need to be reduced or stop due to lactose intolerance. Most lactose intolerance is transitory so breastfeeds could be reintroduced within a few weeks, should the mother maintain her supply through regular expression. I would like to see it strongly stated that allergy should only be diagnosed and treated by a paediatrician and where dietary modification is needed, a dietitian must be seen. 19. Pre-term infants This document occasionally refers to the nutritional management of pre-term infants. As this subject is only briefly touched on there is a danger of providing knowledge without appropriate context. On page 112 it is stated that “Infants weighing less than 2000 g at birth have relatively higher requirements for nutrients, such as protein, calcium, phosphorus and zinc, and often need breastmilk that has been fortified”. I think this subject is 13 actually referring to preterm low birth weight infants, which nutritionally is a very different situation to a term low birth weight infant. The definition for a low birth weight infant is below 2500g, so the use of 2000g here is inconsistent. I suggest that the statement should read pre-term infant weighing less than 2500g and should be referenced. On page 52 it states “women whose babies are in special care should be encouraged –using both practical demonstration and written information – to initiate and maintain an adequate milk supply”. If this specialist subject is to be raised in this document, it may be worth considering putting in some specific advice on how this can be achieved. For example, advice on frequency of expression needed to stimulate supply and the evidence based techniques to improve milk supply through expression [21]. On page 66/7 it is stated “Breastfeeding of premature infants is occasionally supplemented by formula feeding (usually a special product for low-birth weight infants) while in hospital. If these feeds are to be continued after discharge, the mother’s competence in formula preparation and bottle feeding should be ensured and follow-up care organised. In particular, the mother will benefit from information about how she can establish full breastfeeding”. Special products for low birth weight infants that are used in hospital are not available in the community. Instead of saying “if these feeds are to be continued” perhaps, if formula feeds are to be continued, would be more appropriate. Often, if a child is being discharged home from a special care nursery on full or some formula feeds, the chance of a mother being able to then establish full breastfeeds is minimal. The chance of success should be considered before giving a mother advice on how she can establish full breastfeeding to avoid setting her up to fail and causing unnecessary anxiety. 14 REFERENCES 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. Unal, S., et al., Breast-feeding-associated hypernatremia: retrospective analysis of 169 term newborns. Pediatr Int, 2008. 50(1): p. 29-34. Moritz, M.L., et al., Breastfeeding-associated hypernatremia: are we missing the diagnosis? Pediatrics, 2005. 116(3): p. e343-7. Konetzny, G., H.U. Bucher, and R. Arlettaz, Prevention of hypernatraemic dehydration in breastfed newborn infants by daily weighing. Eur J Pediatr, 2009. 168(7): p. 815-8. Wijndaele, K., et al., Determinants of early weaning and use of unmodified cow's milk in infants: a systematic review. J Am Diet Assoc, 2009. 109(12): p. 2017-28. Smith, B.A., Feeding overstrength cows' milk to babies. Br Med J, 1974. 4(5947): p. 741-2. Shaw, J.C., A. Jones, and M. Gunther, Mineral content of brands of milk for infant feeding. Br Med J, 1973. 2(5857): p. 12-5. Wright, C.M., et al., Is baby-led weaning feasible? When do babies first reach out for and eat finger foods? Matern Child Nutr, 2011. 7(1): p. 27-33. Brown, A. and M. Lee, Maternal control of child feeding during the weaning period: differences between mothers following a baby-led or standard weaning approach. Matern Child Health J, 2011. 15(8): p. 1265-71. Brown, A. and M. Lee, A descriptive study investigating the use and nature of baby-led weaning in a UK sample of mothers. Matern Child Nutr, 2011. 7(1): p. 34-47. Davis, A.M., et al., Alpha-lactalbumin-rich infant formula fed to healthy term infants in a multicenter study: plasma essential amino acids and gastrointestinal tolerance. Eur J Clin Nutr, 2008. 62(11): p. 1294-301. Moore, E., Mothers bottle feeding their babies feel negative emotions such as guilt and worry, and receive little information about bottle feeding. Evid Based Nurs, 2010. 13(1): p. 27-8. Lee, E., Health, morality, and infant feeding: British mothers' experiences of formula milk use in the early weeks. Sociol Health Illn, 2007. 29(7): p. 1075-90. Lakshman, R., D. Ogilvie, and K.K. Ong, Mothers' experiences of bottle-feeding: a systematic review of qualitative and quantitative studies. Arch Dis Child, 2009. 94(8): p. 596-601. Sazawal, S., et al., Micronutrient fortified milk improves iron status, anemia and growth among children 1-4 years: a double masked, randomized, controlled trial. PLoS One, 2010. 5(8): p. e12167. Szymlek-Gay, E.A., et al., Food-based strategies improve iron status in toddlers: a randomized controlled trial12. Am J Clin Nutr, 2009. 90(6): p. 1541-51. Becker, G.E., F.M. McCormick, and M.J. Renfrew, Methods of milk expression for lactating women. Cochrane Database Syst Rev, 2008(4): p. CD006170. Rigo, J., et al., Nutritional evaluation of protein hydrolysate formulas. Eur J Clin Nutr, 1995. 49 Suppl 1: p. S26-38. Hernell, O. and B. Lonnerdal, Nutritional evaluation of protein hydrolysate formulas in healthy term infants: plasma amino acids, hematology, and trace elements. Am J Clin Nutr, 2003. 78(2): p. 296-301. Florendo, K.N., et al., Growth in preterm infants fed either a partially hydrolyzed whey or an intact casein/whey preterm infant formula. J Perinatol, 2009. 29(2): p. 106-11. Vandenplas, Y., et al., Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN). J Pediatr Gastroenterol Nutr, 2009. 49(4): p. 498-547. Renfrew, M.J., et al., Breastfeeding promotion for infants in neonatal units: a systematic review and economic analysis. Health Technol Assess, 2009. 13(40): p. 1-146, iii-iv. 15 16