Neonatal Growth and Nutrition
advertisement

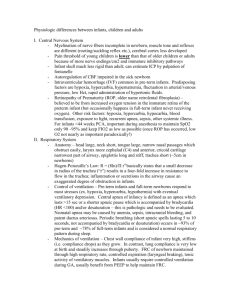
Pediatric Nutrition I Nutrition of Neonates and Infants – Prior to 1 year of age – Growth Rates and Nutritional Goals – Nutrient Requirements Energy, Protein, Minerals, Vitamins Absorptive/Digestive Immaturity – Human Milk – Infant Formulas Growth rates are most rapid in the first six months of human life Nutrient requirements on a weight basis are highest during the first six months Rapid organ growth and development occurs during the last trimester and first six months The detrimental effects of nutritional insufficiencies are magnified during periods of rapid organ growth (I.e., vulnerable periods for brain growth) Provide sufficient macro- and micronutrient delivery to promote normal growth rate and body composition, as assessed by curves which are generated from the population Curves exist for: – Standard anthropometrics: weight, length, OFC – Special anthropometrics: arm circumference, skinfold thickness – Body proportionality: weight/length, mid-arm circumference: head circumference ratio Body composition measurements (e.g. DEXA, PeaPod) are not standardized yet GIRLS Birth to 36 mo BOYS Birth to 36 mo Term infants require 85-90 Kcal/kg/d if breast-fed, 100-105 Kcal//kg/d if formula Differences are due to increased digestibility and absorbability of breast milk – Presence of compensatory enzymes (lipases) (Continued) Energy requirements are 20% higher in premature infants due to: – Higher basal metabolic rate – Lower coefficient of absorption for fat and carbohydrates Energy requirements decrease to 75 Kcal/kg/d between 5-12 months Basal Metabolism Gross Metabolizable Energy Energy Intake Intake Thermic Effect of Feeding Activity Energy Stored “growth” Tissue Synthesis Energy Excretion Diseases of infancy that increase BMR (cardiac, neurologic, respiratory) affect energy requirements Diseases that increase nutrient losses (malabsorption due to cystic fibrosis, celiac disease, short bowel syndrome) increase the need for energy delivery, although the BMR is normal Late gestation and infancy is the time of highest protein accretion in human life Protein requirements range from 1.5 g/kg/d (healthy breast-fed infant) to 3.5 g/kg/d (septic, preterm infant) Amino acid synthesis is incomplete in the premature; taurine and cysteine are additional essential amino acids because of immaturity of enzyme systems Preterm infants: 15 g/kg/d Toddlers: 6 g/kg/d Adolescents: 4 g/kg/d Nutrient Term Preterm 5-12 Month Neonate Neonate Infant Na (mEq/kg/d) 2-3 4-7 1-2 K 1-2 2-4 1-2 Ca (mEq/kg/d) 60 150 40 Iron (mEq/kg/d) 1 2-4 0.7 0.4 0.3 (mEq/kg/d) Zinc (mEq/kg/d) 0.2 - 0.5 Water-soluble vitamins (B, C, folate, etc.) are rarely a problem in newborns and infants; babies are born with adequate stores and/or all food sources have adequate amounts Fat-soluble vitamins (A,E,D,K) may present significant problems because of relatively poor fat absorption by newborn infants (especially premature infants) K: Needs to be given at birth to prevent hemorrhagic disease of newborn; adequate thereafter due to synthesis by intestinal bacteria D: Low amounts in breast milk; infants born in winter in north and infants who are clothed at all times (minimal sun exposure) have been identified with rickets AAP now recommends 400 IU/d for all infants (Continued) A: Essential for normal structural collagen synthesis and retinal development deficiency in premature infants contribute to fibrotic chronic lung disease E: Antioxidant that protects against peroxidation of lipid membranes; preterms have poor antioxidant defense and are subjected to large amounts of oxidant stress; vitamin E deficiency causes severe hemolytic anemia Rapid transit time + Immature digestive capabilities = Reduced nutrient retention Primary sources of CHO in newborn and infant diet are disaccharides (esp. lactose) Disaccharides must be broken into component monosaccharides to be absorbed – Lactose = glucose + galactose (lactase) – Sucrose = glucose + fructose (sucrase) – Maltose = glucose + glucose (maltase) Intestinal lactase concentrations are low at birth and are not inducible Amylase, necessary for breaking down starches, are not adequate until > 4 months Sucrase, Maltase, Isomaltase Glucose Uptake Salivary Amylase Zymogen Granules in Pancreas Pancreatic Amylase Lactose Gluco-amylase 10 Wks 20 Wks 22 Wks 24 Wks 24 - 28 Wks 85 % of ingested protein is absorbed in spite of functional immaturities: – Reduces stomach acidity – Low pancreatic peptides levels (chymotrypsin caroboxypeptidases) Compensation is by trypsin and brush border peptidases Adult: Term 95% infant: 85-95% Preterm infant: 50 - 90% (dependent on source of fat) Low levels of intestinal lipases Small bile salt pool Committee on Nutrition of the AAP strongly recommends breastfeeding for infants The rates of breastfeeding have risen recently, but the attrition rate is high (Continued) The goal of the AAP and NIH Health People 2010 is to have 75% women breastfeed, with a continuation rate of 50% at 6 months It is necessary to breastfeed for at least 12 weeks to achieve the immunologic and disease preventative benefits of breast milk Physician’s role is to support, counsel and trouble-shoot Health Nutritional Immunologic Neurodevelopmental Economic Environmental Studies in developed countries – Reduced prevalence of: Diarrhea » Otitis media » Lower respiratory infection » UTI » NEC (in preterms) » SIDS » Protection of infant from chronic diseases: – Insulin dependent diabetes mellitus (OR 0.61) – Inflammatory bowel disease – Allergic disease – Childhood lymphoma (OR 0.91) – Obesity (OR 0.75-0.87) Protection of mother from: – Pregnancy – Postpartum hemorrhage – Bone demineralization – Ovarian cancer Complete human nutrition for 6 months – Iron at 4 months – Vitamin D in northern climates, covered infants and mothers, vegetarians (vegans) Energy is more accessible than from formula – Compensatory lipases better fat retention – But, BF babies grow slower too Amino acid spectrum matches infant need; lower protein and solute load Faster reflux gastric emptying less Better visual acuity (early) — Role of DHA? Higher IQ (debatable) — Independent of nursing — Components in human milk which may potentiate the effect: » » DHA Growth factors 25% reduced risk of obesity if BF — Adjusted OR: 0.75-0.89 —Dose response (Koletzko et al) — Rate of Adolescent Obesity —12% if BF < 1month —2% if BF 12 months —“Small” effect compared to OR if parents are obese (4.2), low physical activity (3.5) or TV (1.5) Reduced cost of feeding — No formula cost (-$855/year) — Increased maternal consumption (<+$400) — Net savings of >$400/child Reduced health care costs due to: — Lower incidence of childhood illness Reduced income loss due to: — Less days lost to cover childhood illness Galactosemia in infant Illicit drug use by mother Certain maternal infectious diseases — Active TB — HIV (US only) — Not CMV Certain maternal medications — Anti-neoplastics, isotopes, etc — How about SSRI's? Promotes adequate growth, but not brain and immunologic development compared to human milk New formulas contain LC-PUFAs Soon to be added: prebiotics; probiotics Most are cow-milk based, although soy-protein based and fully elemental formulas are available (Continued) Cow’s milk (not formula) is contraindicated in the first year of life — High solute load can lead to azotemia — Inadequate vitamin D and A — Milk fat poorly tolerated — Low in calcium; can lead to neonatal seizures — Gastrointestinal blood loss/sensitization to cowmilk protein Feed humans human milk — It is species specific If not human milk, CMF or Soy formulas with iron are indicated Hypoallergenic formulas are highly specialized, expensive and overused