Establishing State and National POLST
advertisement

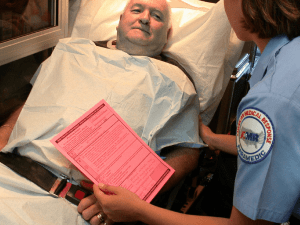
PLEASE NOTE: THIS RESOLUTION WILL BE DEBATED AT THE 2015 COUNCIL MEETING. RESOLUTIONS ARE NOT OFFICIAL UNTIL ADOPTED BY THE COUNCIL AND THE BOARD OF DIRECTORS (AS APPLICABLE). RESOLUTION: 36(15) SUBMITTED BY: Colorado Chapter Florida College of Emergency Physicians New Jersey Chapter Palliative Medicine Section Texas College of Emergency Physicians SUBJECT: Establishing State and National POLST/EOL Registries PURPOSE: Directs ACEP to partner with organizations to advocate for and support creation of state and/or a national POLST/EOL database(s) that can be accessed by emergency physicians; create a task force charged with promoting POLST/EOL registries; exploring cost and regulatory barriers to creating EOL databases, seeking funding options for their creation; consider establishing a database or identifying partners to set up databases; provide a report to the Council in 2016; continue to promote advanced care and end of life planning and coordination as a best practice. FISCAL IMPACT: Budgeted staff resources to explore and advocate for the development of a database. Approximately $15,000 for a task force meeting or related expenses to promote POLST/EOL registries. Additional expenses to retain a consultant may be required to implement the resolution, which could involve significant expense. 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 WHEREAS, The American population is rapidly aging, with an estimated 20% of the U.S. population over the age of 65 by 2050, and many more patients living with complex serious illness; and WHEREAS, Palliative and end of life care is an essential service provided in the ED and will become ever more common in the everyday practice of emergency medicine as our population ages; and WHEREAS, The patient, to the greatest extent possible, should determine the care provided to them, especially while dying or at the end of life; and WHEREAS, Well-recognized programs such as Physician Orders for Life-Sustaining Treatment Paradigm (POLST) exist in some form, often under different acronyms, in 45 of the 50 states, but with great heterogeneity in the services provided; and WHEREAS, Medicare, as of 2016 will compensate physicians for “advanced planning,” leading to a likely boom in the number of completed Advance Directives and POLST forms completed; and WHEREAS, Many patients have end of life wishes documented in POLST, advance directives, or other forms, and due to the acute nature of illness and/or lack of a coordinated medical system, these forms are often unavailable to the Emergency Physicians treating the patient in the ED; and WHEREAS, Emergency Physicians without a POLST form or clear next of kin decision maker are often compelled by current practice standards and malpractice fears to provide care at the end of life that may be futile, costly, and worst of all, against a patient’s documented end of life wishes; and WHEREAS, A system such as the POLST Registry, available only in Oregon at this time, may help physicians know patient wishes and decrease the incidence of futile care or care that violates a patient’s wishes; and Resolution 36(15) Establishing State and National POLST/ EOL Registries Page 2 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61 WHEREAS, POLST forms are of tremendous use to emergency physicians and providers to guide decisions for critically ill patients, that reflect their values; and WHEREAS, A POLST or End-of-Life Registry easily accessible to emergency physicians and medical providers would improve clinical practice, increase certainty around care at the end of life and decrease unwanted and costly futile care; and WHEREAS, ACEP as an organization recognizes the need to improve palliative care in the ED, including it as one of its Choosing Wisely goals and supporting a Palliative Medicine Section; and WHEREAS, Multiple organizations, including but not limited to, the AMA, IOM, AAHPM, and HPNA all advocate for improvements in patient-centered end of life care and coordination and against futile care; and WHEREAS, Other coordinated systems such as Poison Centers and Narcotic Drug Databases, demonstrate that centralized data hubs and knowledge bases are possible, cost efficient service to medical providers and patients; therefore be it RESOLVED, That ACEP partner with organizations such as the American Medical Association, American Academy of Family Physicians, American Academy of Hospice and Palliative Medicine, Hospice and Palliative Nurses Association, AARP, and all others it deems fit to advocate for and support the creation of state and/or a national POLST/EOL database(s) that can be accessed by emergency physicians in times of crisis and uncertainty around a patient’s end of life care; and be it further RESOLVED, That ACEP create a task force charged with promoting POLST/EOL registries, explore the cost and regulatory barriers to creating such databases, seek funding options both internally and externally for the creation of POLST/EOL databases and considers either setting up a database or identifying partners that can set up POLST/EOL databases for the benefit of our members and the American public; and be it further RESOLVED, That the POLST/EOL Registries task force report back to the Council in 2016 with actionable items that the Council, Board, and ACEP can pursue to bring about POLST and end of life databases; and be it further RESOLVED, That ACEP continue to promote advanced care and end of life planning and coordination as a best practice. Background This resolution directs the College to partner with organizations to advocate for and support the creation of state and/or a national Physician Orders for Life-Sustaining Treatment (POLST) and end of life (EOL) database(s) that can be accessed by emergency physicians, to create a task force charged with promoting POLST/EOL registries, exploring cost and regulatory barriers to creating such databases, seeking funding options for the creation of databases, considering setting up a database or identifying partners to set up databases, reporting back to the Council in 2016, and continue to promote advanced care and end of life planning and coordination as a best practice. National Quality Forum The National Quality Forum’s (NQF) 2006 “A National Framework and Preferred Practices for Palliative and Hospice Care Quality,” endorses 38 preferred practices as suitable for implementation by palliative care and hospice programs. Several preferred practices address registries and healthcare and community collaboration. Preferred Practice 34: convert patient treatment goals into medical orders and ensure that the information is transferrable and applicable across care settings. Resolution 36(15) Establishing State and National POLST/ EOL Registries Page 3 Preferred Practice 35: make advanced directives and surrogacy designations across care settings while protecting patient privacy and adherence to HIPAA regulations, for example, by using Internet-based registries or electronic personal health records. Preferred Practice 36: develop healthcare and community collaborations to promote advance care planning and the completion of advance directives for all individuals, for example, the Respecting Choices and Community Conversations on Compassionate Care programs. Registries Several states have end-of-life registry programs, including Louisiana; Montana (stores in secure computer database and makes documents available to providers; Montana code authorizes attorneys general to create and maintain end-of-life registry); and West Virginia (eDirectives Registry available to providers). POLST registries have been implemented in Oregon and a bill is being considered in California. Idaho has a healthcare directive registry and New York has an eMOLST (medical orders for life sustaining treatment) registry. Organizations such as the US Living Will Registry (makes people’s healthcare choices available to their caregivers and families whenever and wherever they are needed while maintaining confidentiality) and Compassion and Choices provide information on each state’s advance directive registry. Resources such as “Electronic Registry Development” from the West Virginia eDirectives Registry and the Archstone Foundation and the Retirement Research Foundation’s “Pathways to POLST Registry Development: Lessons Learned,” provide guidance on establishing POLST registries. ACEP’s End of Life Task Force Recommendations An End of Life Task Force was appointed in 2015 with two primary objectives: 1) catalog existing resources available through ACEP; and 2) make recommendations of additional programs and resources that ACEP could develop. One of the task force’s recommendations is to survey chapters on end of life issues and resources available in each state. ACEP Strategic Plan Reference Goal 1 – Reform and Improve the Delivery System for Emergency Care Objective A – Develop and promote delivery models that provide effective and efficient emergency medical care in different environments. Tactics include: - Develop initiatives and explore partnerships with other healthcare organizations and physicians and policy groups to support improved education for physicians, patients and their families regarding end-oflife decisions. - Engage chapters and other medical organizations to promote Physician Orders for Life Sustaining Treatment (POLST) and other effective advance directive documents. Fiscal Impact Budgeted staff resources to explore and advocate for the development of a database. Approximately $15,000 for a task force meeting or related expenses to promote POLST/EOL registries. Additional expenses to retain a consultant may be required to implement the resolution, which could involve significant expense. Prior Council Action Amended Resolution 21(13) End-of-life Care Public Hearings adopted. Directed ACEP to work with other relevant stakeholders to engage in a national conversation and make recommendations on end-of-life issues. Amended Resolution 31(11) End of Life Care adopted. Directed ACEP to study how emergency medicine can positively affect end of life care, specifically addressing the provision of compassionate and dignified end of life care, and the necessary stewardship of resources; work with other appropriate entities to address patient focused, Resolution 36(15) Establishing State and National POLST/ EOL Registries Page 4 compassionate end of life care; and update the membership regarding actions being taken by ACEP on the important topic of end of life care. Prior Board Action June 2015, reviewed recommendations from the End of Life Task Force regarding current end of life initiatives and resources and discussed additional resources ACEP could develop. Resolution 21(13) End-of-life Care Public Hearings adopted. Resolution 31(11) End-of-life Care adopted. Background Information Prepared by: Marjorie Geist, RN, PhD, CAE Academic Affairs Director Reviewed By: Kevin Klauer, DO, EJD, FACEP, Speaker James Cusick, MD, FACEP, Vice Speaker Dean Wilkerson, JD, MBA, CAE, Council Secretary and Executive Director