ER-POLST
advertisement
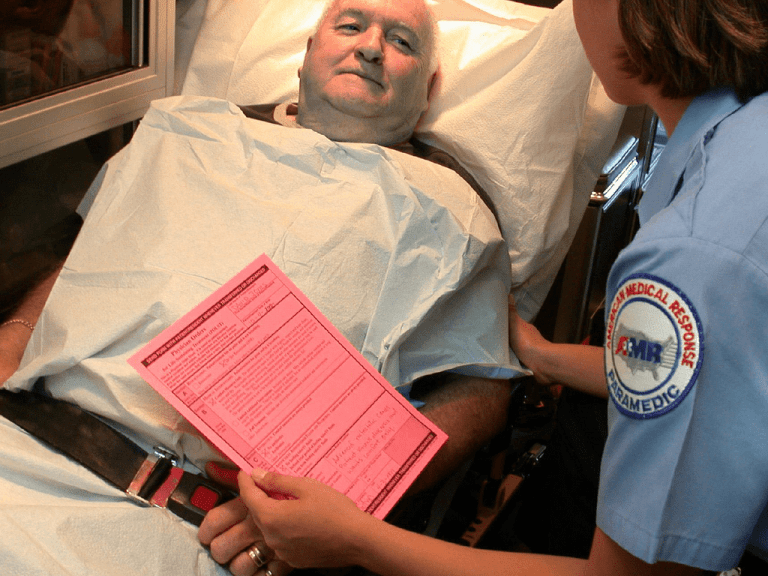
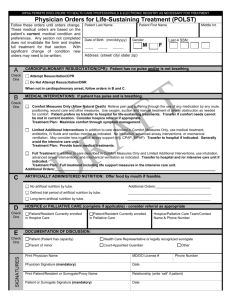
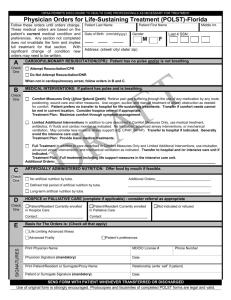
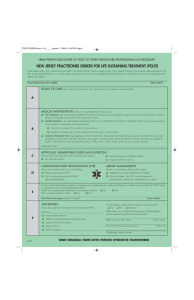
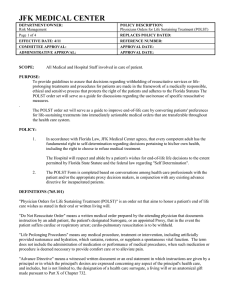
Palliative care and POLST in the emergency department Terri Schmidt MD, MS Professor of Emergency Attending Inpatient Palliative Medicine Team OHSU February, 2012 Goals of Care • What were you hoping would happen when you came to the emergency department today? • What has your doctor told you about what you can expect in the future? “If I have cancer or something, [resuscitation] is a waste of time, because you know you’re going to die. I would like to be in a hospice situation where there is someone to hold your hand or make sure you are comfortable.” ED Palliative Medicine Consults • In house Monday through Friday 9am to 5 pm • After 5 pm by phone Monday through Thursday (Goal 24/7) • Consider admission to OBS with am consult (can put electronic order request in EPIC) • Inpatient & Ed consults: Eric Walsh MD, Paul Bascom MD, Terri Schmidt MD, Mary Denise Smith Advance Practice Nurse • Outpatient appointments: Eric Fromme MD, Paul Bascom MD Emergency Rule patient lacks decision capacity no one legally authorized to act for patient is available serious risk of bodily injury or death if a decision is not made quickly a reasonable person would consent Surrogate decision makers • Standard – Patient expressed preferences – Best interest • Hierarchy – Legally appointed guardian – Durable power of attorney for health care – Spouse or partner of a registered domestic union – Majority of adult children – Parent – Majority of adult siblings – Other friend or relative – Attending physician Determining capacity Risks and benefits explained to patient Patient understand risks and benefits Make decision based on life values and goals Consistent over time ability to communicate a decision • Reassess for each decision ED physician & non-beneficial • No obligation to provide non-beneficial interventions • Based on goal of intervention Definitions • Advance directives – Directive to physicians/living will – Power of attorney for health care • Do not attempt resuscitation-DNAR • POLST and POLST paradigm ADVANCE DIRECTIVE POLST For whom For all adults Purpose To express values and Medical orders which appoint a surrogate turn a patient’s values (future wishes) For persons of any age with advanced illness into action (applies today) Guide actions by Usually not Emergency Medical Personnel Guide treatment Yes decisions in the hospital Yes Yes What Is POLST • A health care provider’s order • Can be completed by others (SW, RN) but must be signed by MD, DO, NP or PA – May be a verbal order from one of the above, signed by an RN • Consistent recognized document Development of POLST • • • • Consensus development Began in 1991 Newest revision June 2011 Voluntary process in Oregon, legislated in some other states including Washington • Endorsed programs in 12 states and developing in over 30 • National POLST Taskforce “If I am unconscious at the last moment then I don’t want any machines or anything.” Oregon Rules •EMT Scope of Practice [OAR 847-35-0030(6)]. – The Oregon Medical Board has defined the Scope of Practice so that an Oregon-certified First Responder or EMT shall comply with lifesustaining treatment orders executed by a physician, physician assistant or nurse practitioner •Oregon Medical Board [OAR 847-010-0110] – The fact that a physician, physician assistant or nurse practitioner who executed a life-sustaining treatment order does not have admitting privileges at a hospital or health care facility where the patient is being treated does not remove the obligation under this section to honor the order.” – Mandate for signers to enter POLST into Registry unless patient opts out. Completion of a form is voluntary Requirements for a Form Valid • Patient name • Resuscitation orders • Health professional signature and date all other information is optional…in Oregon it does not require signature of patient (verbal orders signed by an RN are acceptable) Section A: Cardiopulmonary Resuscitation (CPR) 5/19/2011 Section B Medical Interventions 4/9/2015 Section C ARTIFICIALLY ADMINISTERED NUTRITION 4/9/2015 Section D DOCUMENTATION OF DISCUSSION 4/9/2015 SIGNATURES 4/9/2015 Legal case • Can I be liable for not honoring a form? • California case • Case filed against an ED physician for not honoring a POLST order to not intubate Difficult situations • Family conflict • How do you interpret Attempt Resuscitation and Limited Interventions? • Trauma Suicide • Emergency physicians may be required to care for patients at the end-of-life who attempt suicide (without physician assistance) • Physicians should counter the medical effects of suicide attempt unless such measures would only prolong the dying process or would be ineffective The Oregon POLST Registry Emergency Medical Services, emergency departments and hospital acute care units What is it? • Secure electronic registry of POLST orders. • Located at the Emergency Communication Center at OHSU and protected by the OHSU firewall • Allows health care professionals access to POLST orders if the original POLST form cannot be immediately located • Over 80,000 forms currently in Registry • Entering about 3200 new forms/month Calls as of January 31, 2012 • 1085 calls • 335 matches • 31% match rate Reasons for Calls 12/3/2009 to 8/31/2010 • 183 EMS the Registry • 93 calls (51%) were for patients with trauma, SOB, acute illness but not arrest • 38 calls (21%) patients in cardiac arrest • 16 calls (9%) patients with terminal illness • 3 calls (1%) were patients in respiratory arrest Users • Emergency departments 46% • EMS 36% • Acute care 17% How to access the a POLST in the Registry • Call the ECC (4-7551 or 4-7333) • They need enough info to accurately ID patient (usually can get it from EPIC •Name •Date of Birth •Gender •Last 4 SSN •POLST Registry ID # •Address Pain Management • Trick of the trade Free IPhone app: Opioids Equianalgesic doses of opioid analgesics Morphine (MS) 1 mg IV = 3 mg po MS 30 mg po = oxycodone 20-30 mg po Hydromorphone 1mg IV = MS 7 mg IV MS 5 mg IV = fentanyl 50 mcg . . . Changing opioids • Cross-tolerance – start with 50%–75% of equianalgesic dose • more if pain not well controlled, less if adverse effects Breakthrough dosing • Use immediate-release opioids – 5%–15% of 24-h dose • Do NOT use extended-release opioids • Avoid acetaminophen toxicity Allergy vs. adverse effect • Opioid-induced nausea/vomiting, constipation, drowsiness, confusion are NOT allergic reactions • Anaphylaxis, urticaria, pruritus with rash but RARE • If true allergic reaction, replace with opioid of a different class Urticaria, pruritus (no rash) • Morphine, hydromorphone, usually not fentanyl • Mast cell destabilization followed by histamine release • Manage with antihistamines or change to fentanyl Trick of the trade…pain crisis • Morphine 1 mg IV q minute to total 10 mg, monitoring at bedside for effect, somnolence, respiratory depression • Wait 10 minutes • Repeat until satisfactory pain control (Alternatives hydromorphone .2 mg or fentanyl 20 mcg) Pathophysiology nausea/vomiting Antiemetics • Dopamine antagonists: haloperidol, prochlorperazine, droperidol, promethazine, metoclopramide (also prokinetic) • Antihistamine: diphenhydramine • Anticholinergic: Scopolamine • Serotonin antagonists: ondansetron, granisetron • Other: dexamethasone, THC, lorazepam Trick of the trade: Haloperidol is a great antiemetic! Antacids • H2 receptor antagonists – cimetidine – famotidine – ranitidine • Proton pump inhibitors – omeprazole – lansoprazole • Misoprostol POLST Information Center for Ethics in Health Care, OHSU • 503 494-3965 • Fax: 503 494-1260 • Ethics@ohsu.edu • www.polst.org