The Patient`s got a POLST…now what?
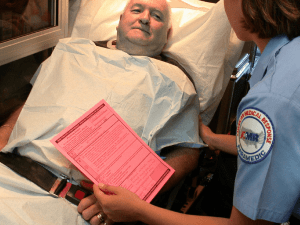
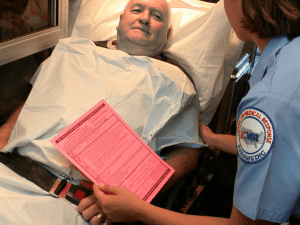
advertisement

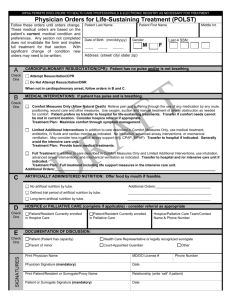
Treating the person with a POLST in crisis Purpose of POLST To provide a mechanism to communicate patient preferences for end-of-life treatment across treatment settings Patient Primary Care Provider Care facility Emergency Medical Services Hospital Clinic/Specialist POLST Basics What do you look for first? Patient name MD/DO/PA or NP signature ○ Is there a T/O or V/O (verbal orders) signed by an RN? --these are ok! Date signed If the above criteria are not met, the form is not a valid medical order Onto the orders Section A: Cardiopulmonary Resuscitation When does section A apply? ○ ONLY when the patient is NOT breathing AND is pulseless. Section A POLST-isms “Until they die, it doesn’t apply” “Once they’re dead, go ahead” Section B: Medical Interventions When does section B apply? When the patient still has a PULSE and/or is still BREATHING Section B POLST-isms “Heart’s got a beat? See Section B for how to treat!” “Is the patient still breathing? Then interventions they’ll be receiving” Section B: Comfort Measures Only Do: any intervention that will help keep the patient comfortable Do: Try to resolve care concerns that are manageable by the providers on scene If the issue becomes larger, consider calling OLMC Consider transporting only when the patient cannot be kept comfortable at their primary location Does not mean do not treat! Section B: Limited Additional Interventions Do simple, minimally invasive interventions Avoid intubation Do: Transport if there is a simple medical intervention that can be provided by the ED or hospital Section B: Full Treatment Treat as per your standard of care for that particular condition! Scenario 1: EMS arrives at the home of a 78yom c/o SOB, GCS 15. Pt’s son is on scene and presents you with a POLST that is signed by the physician but bears no patient signature. PMH: COPD, HTN Can you follow the orders? Form states DNR, Limited Additional Interventions Which order is most relevant in the patients’ current medical state? What treatments would you consider? Scenario 2: POLST & the CA pt Arrive on scene of a 52 year old woman, thin and ill- appearing with metastatic breast cancer. She is c/o new onset nausea and pain in her jaw. What else do you need to know? Before seeing a POLST form what treatments are you considering? Scenario 2: 12-lead results Kern, Morton MD “The Different Presentations of Acute STEMI: What Problems Should the Cath Lab Look For?” 12/30/10; www.cathlabdigest.com Now what? Do you transport? Would your decision to transport change if you were able to control the patient’s pain on scene? If you decide to transport where do you transport to? What info should you relay to the receiving hospital besides that this is a STEMI patient? Quiz time! Can you follow POLST orders that are from a different state than Oregon? Yes! (Question… contact OLMC) Are copies of POLST form ok?? Yes! Scenario #3 72yom, general malaise who stated “I just don’t feel right.” What is the first thing you need to find out? The patient is awake and c/o CP & SOB. Monitor shows V-tach Treatments? You decide you’d like to cardiovert What do you explain to the patient? Cardiovert asystole Now what? Quiz time! When do you consider using CPAP on the patient with a POLST order of CMO? The patient has to be alert enough to cooperate in order to try CPAP. Is it helping? ○ Yes—then this is a comfort measure ○ No—then take it off, and try something else Scenario 4: I’ve fallen and I can’t get up! 88 year old woman falls at care facility. GCS13. BP 94/70, P 96; unstable pelvis. RN on scene hands you POLST form: DNR, CMO Does the POLST form influence your decision to transport? Does it change the destination? It’s easy! When should I call? Elderly, frail patients Terminally ill patients Chronic, progressive illness patients If someone states there may be a POLST but cannot provide a copy If you are not certain the POLST for you have is current What is the Oregon POLST Registry? Secure electronic database of POLST forms. Owned by the state of Oregon, operated by the Emergency Communication Center at OHSU and available statewide. Emergency medical professionals treating a patient can access POLST orders if the original POLST form cannot be immediately located. How do I access the POLST Registry? For emergent needs • – Call the POLST Registry EMS Hotline* State: “This is <your name & title> from<Agency name>, with a POLST form request” Provide some of the following patient identifiers, as requested by the Registry Hotline staff: •Full name •Date of Birth •Gender •Last 4 SSN •POLST Registry ID # •Home address/residential care facility address •City, County, or zip code *this number is available for EMS, ED and acute care hospital unit use ONLY. It is not for public distribution or dissemination Do I need to have all those identifiers? NO! If possible, start with these identifiers Registry ID ○ This may be present in a person’s personal effects on a bright pink sticker (example right) Date of Birth First and last name Hotline staff may request additional identifiers to confirm the identity of a patient What information will be provided? • The Registry staff can verbally relay: • Section A and B orders • Date the form was signed • Patient’s POLST Registry ID • THE STAFF ARE NOT MEDICAL PROVIDERS, AND CANNOT INTERPRET POLST ORDERS • If you need guidance, contact On-Line Medical Control Transporting? Let us know! We will fax a copy of the POLST to your destination hospital What do I document? Verbal orders relayed Example: DNR; Limited additional interventions Date the form was signed POLST Registry ID You can always call the business office and request a copy of the POLST for your chart. Calls received after hours will be faxed the next business day The Oregon POLST Registry Office EMS Contact Jenny Cook, Oregon POLST Registry Liaison Call for any non-urgent questions, or educational information or onsite training requests. Phone: 503-494-1230 Toll free: 877-367-7657 Fax: 503-418-2161 E-mail: polstreg@ohsu.edu Website: www.orpolstregistry.org