Instrument-II-NC-MOST-Research-Presentation-Poster
advertisement

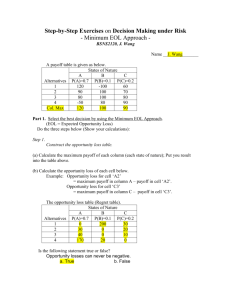
Increasing Residency Training of Goal-oriented Treatment Options in Patients with Life-limiting Illnesses Poster Tae Joon Lee, Qing Cao, Stella Hayes, Phillip Austin, Muhammad Zafar, Shiv Patil, Robert Newman Qing Cao, MD, HRSA 1-K01 HP20471 Geriatric Academic Career Award . The investigators retain full independence in the conduct of this research A80 East Carolina University, Greenville, North Carolina Abstract Objectives: For many patients with life-limiting illnesses, defining and discussing goals of future medical care (advance care planning) are very important. This study measures the effects of education to the in-training residents of family medicine (FM) and internal medicine (IM) residency programs at East Carolina University (ECU). Sample Educational Material Conclusions: Educational sessions significantly impacted residents’ knowledge and attitude about advance care planning and EOL care. Background Most seriously ill patients are not able to make decisions at the end of life Surrogate decision maker to patient concordance about treatment preferences is often poor Improvement of surrogate understanding of patient preferences has the potential to improve both patient and surrogate outcomes Structured, facilitated patient-surrogate conversations are associated with improved surrogate understanding of patient wishes. Resident physician training in discussion of goaloriented treatment options is not standardized. Alive 8% Attitude Test Score Goals of Care: Alive Dead Dead 92% Design: Based on the results of the informal assessment of need from the residents and faculty, educational materials were developed. These included discussion of advance care planning, MOST (POLST) form, FIVE WISHES, healthcare power of attorney, and living will. A 2-hour education and discussion session was given to all in-training FM and IM residents at ECU. Pre- and post-tests were administered to measure their medical knowledge as well as attitudes toward advance care planning. Results: A total of 70 pre-test and 53 post-test scores were analyzed. Overall knowledge improved with the educational sessions (74.9% vs 90.5% correctly answered pre- and post-test, respectively). Also, the residents’ own attitude toward advance care planning changed favoring less aggressive care at the end-of-life (EOL). Results Survival After Un-witnessed CPR Alzheimer’s Dementia Diagnosed Overall Attitude Knowledge Scores Pre Test 33% Overall Knowledge 75% 91% <0.00 1 41% 0.037 Which EOL planning tools do you know about? 77% 92% <0.00 1 In which order can the following individuals make medical decisions if a patient is incapable? 56% 89% <0.00 1 How many patients with a witnessed cardiac arrest survive CPR? 84% 91% <0.00 1 If pneumonia is not treated with antibiotics, does this increase discomfort level for patients with advanced dementia? 64% 85% 0.017 Whether to treat infections at EOL 24% 40% 0.095 Location of care at EOL 52% 69% 0.090 Interest in advanced 6 directives 62% 75% 0.197 Whether to use tube feeding at EOL 63% 58% 0.245 Whether use IV fluids at EOL 19% 27% 0.543 How many patients with advanced illnesses who get CPR in the hospital survive? 79% 93% 0.057 Desire CPR 10% 15% 0.578 Does tube feeding eliminate the risk of aspiration pneumonia for patients with advanced dementia? 90% 94% 0.643 5 4 Average Years Until Death 3 2 1 0 At age 60- At age 70- At age 80- At age 90 or 69 79 89 older Age (yr) Patients with In-Hospital CPR number (percent) Survival to Hospital Discharge percent (95%CI) 65-69 63,299 (14.6) 22.2 (21.9-22.6) 70-74 84,353 (19.4) 20.9 (20.6-21.1) 75-79 98,263 (22.6) 19.1 (18.9-19.3) 80-84 91,471 (21.1) 17.0 (16.8-17.3) 85-89 62,530 (14.4) 15.1 (14.8-15.4) >=90 34,069 (6.9) 12.2 (11.9-12.6) Yes 10,924 (2.5) 11.5 (10.9-12.1) No 423,061 (97.5) 18.5 (18.4-18.6) Admitted from a SNF Methods Based on the results of the informal assessment of need from the residents and faculty, 2-hour educational materials were developed. These included discussion of advance care planning, MOST (POLST) form, FIVE WISHES, healthcare power of attorney, and living will. Pre- and post-tests were administered to measure their medical knowledge as well as attitudes toward advance care planning. Postp test value Post p Test value 8 7 PreTest Resident comments: 1. Not enough time 2. Family or patient did not want to talk about end of life issues or code status 3. Resident is not familiar with resources available (still not sure how to use MOST, living will, 5 wishes, etc) Conclusion Educational sessions significantly impacted residents’ knowledge and attitude about advance care planning and EOL care. Some residents felt more comfortable with discussion regarding goals of care, MOST (POLST) form use, advance directives, HCPOA, and living will. Time and training are significant factors in residents’ ability to discuss these issues with patients. More targeted educational opportunities and longer follow up are needed and need to be standardized in medical training. References CPR & Sudden Cardiac Arrest (SCA), Fact Sheet, as of April 26, 2010. Epidemiologic Study of In-Hospital Cardiopulmonary Resuscitation in the Elderly, The New England Journal of Medicine Jul 2, 2009. Vol. 361, Iss. 1; pg. 22 One-year trajectories of care and resource utilization for recipients of prolonged mechanical ventilation: A cohort study, Unroe M, Tulsky JA, Cox CE, Ann Intern Med 2010 153:167-75 Survival of people with clinical diagnosis of dementia in primary care: cohort study, BMJ 2010; 341:c3584 doi: 10.1136/bmj.c3584 (Published 5 August 2010), Cite this as: BMJ 2010; 341:c3584 Survival and comfort after treatment of pneumonia in advanced dementia, Arch Intern Med. 2010 Jul 12;170(13):1102-7 Survival analysis in percutaneous endoscopic gastrostomy feeding: a worse outcome in patients with dementia, The American Journal of Gastroenterology (2000) 95, 1472– 1475