Acoustic Reflex Magnitude and Growth
advertisement

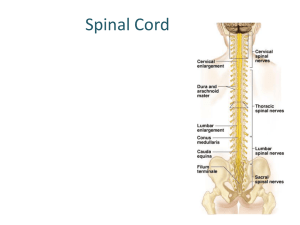
Acoustic Reflex 2004-06-16 R3 施偉勛 Anatomy of Intratympanic Muscles 1. Stapedius muscle ---innervated by CN VII ---the smallest skeletal muscle, 6 mm long, 5 mm2 in cross section ---completely inside a bony canal within the pyramidal eminence ---insert on the posterior surface of the neck of the stapes, above post crus ---pull the stapes in the posterior direction 2. Tensor tympani muscle ---innervated by CN V, 25 mm long, 5.85 mm2 in cross section ---inside the tensor tympani semicanal above the Eustachian tube ---exit the middle ear wall, making a turn around the cochleariform process ---ending at the top of the manubrium of the malleus ---pull malleus anteriorly and medially ---contraction in startle response # both muscles exert forces on the ossicles perpendicular to their normal manner of rotation siffen the middle ear transmission system, impedance # activate by vocalization (stapedius contraction before vocalization), chewing and yawning, tactile and similar stimulation of the ears and face Acoustic Reflex, from one or both of intratympanic muscle # observation through perforated eardrum: stapedius m action (Luscher 1929) # Terkildsen (1960): monitor changes in air pressure in ear canal ---stapedius contraction: outward movement of the drum ---tensor contraction: pull the drum inward # AR (+) in tensor pathology (Jepsen 1955) Acoustic Reflex Pathways (Borg 1973, Lyons 1978, Fig ) # Disorder superior to the reflex pathway do not affect AR, ex cortical lesioin # abnormal AR in demyelinating dz, ex. MS, and neuromuscular dz, ex. MG Nonacoustic Reflex # elicited by tactile or electrocutaneous stimulation of the face and around the pinna (stapedius m) # stimulate the orbital area (startle response): activate both middle ear m. 1 # CN V, VII, IX, X nucleus of solitary fasciculus reflex center in dorsolateral reticular formation CN VII motor nucleus # If AR (-), and nonacoustic reflex (+): afferent (sensory) abnormality If AR (-), and nonacoustic reflex (-): efferent (motor) abnormality Contralateral vs Ipsilateral 1. advantages in contralateral AR 1) sensitive to disorder involving the crossed reflex pathways (eg. Intra-axial lesion) 2) less susceptible to artifact than ipsilateral AR: by multiplexing circuit 3) more extensive normative data are available for contralateral tests 2. advantages in ipsilateral AR 1) sensitive to middle ear pathology, not influenced by the opposite ear dz 2) possible in difficult-to-test p’ts that precludes the use of the headset 3) avoid collapsed ear canal artifacts Biphasic responses (Hung and Dallos 1972) # impedance at onset: reduction in resistance occurs at the onset of the reflex response as the muscle contraction momentarily changes the coupling between the stapedius footplate and the cochlear fluid # biphasic at onset and offset: ---early stage in otosclerosis, congenital stapes fixation, osteogenesis imperfacta ---elasticity changes in the stapes and annular ligament ---(+) in normal ears when probe-tone in 600-700 Hz, in otosclerosis at all frequency Acoustic Reflex Threshold (ART) # lowest level of a sound stimulus that elicits an AR response # stimuli: 500, 1000, 2000 Hz and broadband noise (BBN) # 4k: not recommended, ART in normal-hearing young p’t (rapid adaptation) # not affected by the direction in which the stimulus level is changed, but ART lower with descending method than with ascending method (Jepsen 1963) # 5-dB steps in pure tone vs 1 or 2-dB in BBN 2 Normal Acoustic Reflex Thresholds # 85 to 100 dB SPL for puretone stimuli, 20 dB lower for BBN ( Fig ) # 3dB lower for ipsilateral than contralateral # normal 20 dB noise-tone difference in two youngest group # BBN ARTs with 5 dB step > with 1 dB step # critical bandwidth: beyond this bandwidth result in lower threshold (Fig ---the width of the critical band increases with center frequency ) 1. Effects of aging ---tonal ART do not change with increasing age in normal-hearing adults ---ART for BBN do increase with increase age (breakpoint at 44 y/o, Fig ) 2. AR in Newborns ---probe tone (220 or 226 Hz): high proportion of absent AR or elevated AR ---higher frequency probe: better ART, ipsilateral > contralateral (Table ) ---as age , ART , but more for tones than for noise (6dB from 2 d/o to 6 w/o) 3. Conductive Disorders ---probe ear principle: AR absent when conductive pathology in probe ear; AR(+) in 50% when ABG=5 dB (Jerger 1974) ---stimulus ear principle: ART by the amount of the ABG, and absent if elevated beyond the maximum stimulus level (ABG: 42 dB, Max: 125 dB) ---AR (+) in 50% when ABG=27 dB in stimulus ear (Jerger 1974, Max: 110dB) ---ipsilateral is sensitive to conductive disorder due to double effect ---ossicular chain discontinuity: lateral to stapedius m absent AR paradoxical finding when 1) bridged by connective tissue, ex: fibrous adhesion 2) disruption is medial to the stapedius m. insertion ---Criteria for middle ear disorder: Sen 90%; Spec 92.5% ( Silman 1992) A. Tympanometric criteria ( 50 dapa/sec pump speed) 1) tympanometric width of > 180 dapa, and/or 2) static middle ear admittance of < 0.35 mmhos, and/or 3) tympanometric peak pressure of ≦ 100 dapa, plus B. absent ipsilateral AR for 1000 Hz at 110 dB HL (with multiplexing) 4. Sensory-Neural Disorder (Fig ) ---puretone ART: constant until up to 50 dB HL ---ART for BBN: higher as the HL increase up to 50 dB, then constant ---large-sample norms for contralateral ART (Fig ); none for ipslateral 5. Retrocochlear Disorder ---elevated ART (>90% percentile) above the ART in normal or cochlear-impaired ears, or absent at the maximum stimulus 3 ---conductive disorder must be ruled out ---positive reflex decay ---inter-ear ART comparison: > 15 dB at more than one frequency (Chiveralls, 1977), > 10 dB at two adjacent frequencies ( Prasher & Cohen 1993) sen # >90% ART + decay AR: 85% sen in retrocochlear lesion Temporal Summation (Fig ) # stimulus duration less than 1 sec # 10-fold decrease in duration was offset by a 20-25 dB increase in signal level (time-intensity trade) ( Djupesland 1973) Loudness recruitment # loudness: the perceptual correlate of the intensity of the acoustic stimulus # loudness increases as stimulus level is increased # Loudness recruitment: As the signal above the impaired threshold, the loundness grows as a faster rate than normal in response to increasing stimulus level # Metz (1952): ART at lower sensation level from p’t with SNHL AR was elicited by the loudness of the signal. Lower SL of AR reflected recruitment #Jepsen (1963): auditory threshold with age, the ART tended to decrease Acoustic Reflex and Middle Ear Transmission # When m. contraction, PTA was shifted by 20-40 dB at 125-500 Hz, and by 15 dB at 1000 Hz, little change at higher frequency (Smith 1943, Reger 1960) # AR affect the frequencies below about 2000 Hz by changes in cochlear microphonic magnitude (Moller 1965) Acoustic Reflex Decay (Adaptation) # reduction in the magnitude (≦ 50%) of the AR during the sustained stimulus # for 10 sec at a level 10 dB above the ART in contralateral # limit to 500 and 1000; rapid adaptation of AR in higher frequencies (Fig ) # in D/D retrocochlear lesion: decay AR in 500 Hz better than in 1000 Hz, in first 5 seconds better than in second 5 seconds # in 1000 Hz with ≧ 50% AR decay within 5 sec and ≦ 50% decay in 6-10 sec: 99% specificity ( Ferguson 1996) Acoustic Reflex Magnitude and Growth # AR magnitude as the stimulus above ART 4 # Acoustic reflex growth function: describe this relationship ( Fig ) ---for puretone (85-120 dB): linear change ---for BBN (70-110 dB): two segment; curvilinear tail # reduce by aging, CN 8 and brainstem pathology # inter-ear magnitude comparison: < 0.75 in CN 8 tumor as at 10 dB SL re Acoustic Reflex Latency (ARL) (Table ) # 150 msec at 80 dB sensation level to 40 msec at 100 dB SL (Metz 1951) # as short as 12 ms by EMG in stapedius m (Zakrisson, Borg 1974) # ARL shorter as the stimulus level increases (20-<300 ms) (Bosatra 1984) # earliest reflex latency within 95% normal ranges: 51 ms (Qiu, Stucker 1997) # ARL similar for normal through the fifties, with increasing age in the sixties # within normal range with cochlear disorder, but > 200ms in retrocochlear dz # not provide diagnostically useful information in central auditory pathology # D/D: additive or subtractive artifact: 0 ms ( no latency) Drug Influence 1. Barbiturates: ---produce elevated ART, greater effect contralaterally than ipsilaterally ---increase in AR latency (Bosatra 1984) 2. Ethyl alcohol ---elevated ART, similar for both contralateral and ipsilateral --- ART larger for broacband noise than for pure-tone stimuli --- incidence of absent AR among alcoholics ( Spitzer & Ventry 1980) 3. Antipsychotic drug chlorpromazine --- ART (Simon & Pirsig 1973) Hearing Loss Identification and Prediction # identify the HL existence than try to predict the amount of HL (lack precision) # noise-tone difference in ART: smaller as HL up to 50 dB, then larger again # bivariate approach by Popelka and Trumph 1976 ( Fig ) ---≧ 90% of normal young ears in the left area ---young patient with PTA ≧ 32 dB in the right region Reflex Theories 1. Protection theory ---weakened by 1. AR latency; 2. AR adaptation; 3. sound intense enough to 5 elicit AR are virtually nonexistent in nature ---beneficial side effect of AR 2. Fixation theory ---keep the ossicles in proper position 3. Perceptual theory ( Simmons 1964) # a sharp antiresonance peak at 4k Hz in cats without intratympanic muscle, as well as in normal cats under anesthesia ---frequency response of the conductive mechanism is smoothed by the tonus of the intratympanic muscles ---modulation of the muscle tonus improves attention to the acoustic environment ( as extrocular muscles in vision) ---attenuate the low-frequency internal sounds, improve signal-to-noise ratio 4. multifunctional theory (Borg 1976) ---prevent from desensitization: reduce unimportant sound ex: eating, talking, yelling ---prevent from interference: attenuated the low frequency of speech that wound otherwise mask the higher frequency, improve dynamic range ---prevent from injury: attenuation of intense sound Reference 1. Gelfand SA: The Acoustic Reflex. In Katz J: Handbook of clinical audiology, 5th ed. Maryland, Lippincott Williams & Wilkins, 2002, pp 205-232 2. Gelfand SA: Conductive Mechanism, Hearing: an introduction to psychological and physiological acoustics, 3rd ed. New York, Marcel Dekker INC, 1998, pp 101-119 3. Djupesland G: The Acoustic Reflex. In Jerger J, Northern JL: Clinical impedance audiometry, 2nd ed. Massachusetts, American Eletromedics Corp, 1980, pp 65-79 5. Simmons FB, Calif PA: Perceptual theories of middle ear muscle function. Ann Otol 1964; 73: 724-740 6. Vincent VL, Gerber SE: Early development of the acoustic reflex. Audiology 1987; 26: 356-362 7. Stach BA: The Acoustic reflex in diagnostic audiology: from Mets to Present. Ear and Hearing 1987, suppl 8: 36-42 8. Johnson KC: Audiologic assessment of children with suspected hearing loss. Otolaryngol Clin N Am 2002, 35: 711-732 9. Moller AR: Auditory Neurophysiology. J Clin Neurophysiol 1994, 11: 284-308 10. Margolis RH: Detection of hearing impairment with the acoustic stapedius reflex. Ear and Hearing 1993, 14: 3-10 6