MCTD case - Warren Prokopiw
advertisement

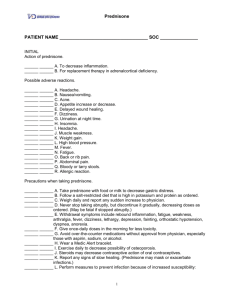
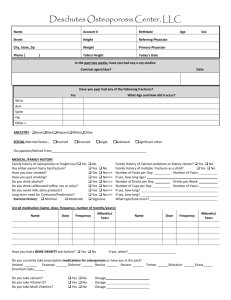
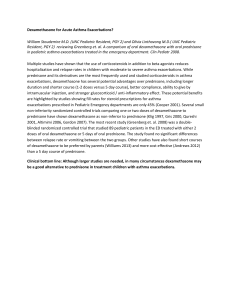
Mixed Connective Tissue Disease Warren Prokopiw Resident 2011-2012 Outline • • • • • • • • • Past History Current Medication History Clinical Course All DRPs Summary on Mixed Connective Tissue Disease Goal of Treatment Recommendations and rationale Monitoring Actions and Follow up Patient Information • • • • • SH is a 41 or female Married, 2 children, on disability Social smoker, quit 18 years ago Non-drinker, used to smoke marijana NKDA Chief Complaint / HPI • Abdominal pain, nausea, vomiting • • • • • Partial L nephrectomy 13 Sep - Disch 18 Sep Night sweats day after discharge Increasing fatigue, and sweats Presented to ER on 22 Sep T36.8, BP 168/108, HR 105 – Urinalysis – protinuria, 10-40 RBC • Bilateral pyelonehprtitis – Cefriaxone 1g IV Q24 Previous Medical/medication History • Anxeity/ panic disorder – Paroxetine 40 mg daily • Systemic Lupus erythematosus – mostly affecting joints – Methotrexate 10 mg q Thurs – last dose 8 Sep – Prednisone 20 mg x 5 days 1 year ago • Nehrolithiasis – calyceal diverticulum with stones – Partial nephrectomy • L uteric stent 2001 • 20 Sep - Cephalexin 500 QID and Tylenol #3 Clinical Course • Persistent fever and Tacycardia – added Cipro 400 IV Q12H, then changed to imipenem 500 IV Q6H • Cultures – blood negative, urine candidia – Changed to fluconazole 200 mg PO daily • 2 Oct – pleuritic chest pain/SOB, ST Elevation <1mm ? PE and antiphospholipid syndrome • MCTD myopericarditis – Methylprednisolone 60 mg IV Q8H to Prednisone Review of systems • • • • Vitals T 36.2, BP 111/83, HR 78, R 18, 98% RA EENT – dipoplia Resp – chest clear, CT Chest – No PE CVS – S1S2 normal, no pericardial rub, JVP normal • Abdomen – soft, nontender, complaint of GI upset • Skin – improving Janeway lesions, remaining splinter hemorrhages Splinter Hemorrhages Janeway lesions Labs • • • • • • WBC 12.3, Hg 90, RDW 15.3, Neut 11.39 Scr 38, eGfr > 120 CRP 16.7 (down from 121.4) AST 40, ALT 12, AlkP 149 Trop + ANA +, RNP +, Cardiolipin IgG 31, IgM 17 Current Medications • • • • • • • • • • • • • Zopiclone 3.75 – 7 mg QHS Paroxetine 20 mg daily Lorazepam 1 mg PO/SL TID prn ASA 162 mg daliy Heparin 5000 U Subcut Q12H Nitroglycerin 0.3 mg pumpspray prn Metoprolol 6.25 mg BID Esomeprazole 40 mg daily Cardiac bowel protocol Ferrous Fumarate 300 mg BID – Folic Acid 1 mg daily Prednisone 50 mg QAM Tramacet 1-2 tabs TID prn Acetaminophen 0.5 – 1 g QID prn Drug Related Problems • SS is experiencing a flare in her MCTD due to lack of suppressive therapy • SS is experiencing GI upset as an adverse effect of prednisone treatment • SS is at risk of worsening anxiety due to lowered paroxetine dose • SS is at risk of osteoporosis from recurrent steroid use • SS is at risk of stomatitis or hepatotoxicity as an adverse effect of methotrexate treatment Mixed Connective Tissue Disease • Autoimmune disease against own connective tissues • considered an overlap of – SLE, scleroderma, polymyositis • 2.7 cases per 100,000 • Female 10:1 over males • Typical onset age 15-25 MCTD Symptoms • Common Symptoms – Raynaud phenomenon, swollen hands, – anti–U1-RNP antibodies (hallmark) • SLE findings – Polyarthritis, Lymphadenopathy, Facial erythema, Pericarditis or pleuritis, Leukopenia or thrombocytopenia • Scleroderma findings – Sclerodactyly, Pulmonary fibrosis, esophageal hypomotility • Polymyositis findings – Muscle weakness, elevated serum muscle enzymes Raynaud phenomenon Goals of Treatment • No RTCs to guide therapy – Management based on therapies for SLE, scleroderma, or polymyositis • Control symptoms and maintain function – Target medical therapy to specific organ involvement – Minimize glucocorticoid burden • hydroxychloroquine 400 mg daily • methotrexate 7.5 -15 mg per week – Monitor for development of pulmonary hypertension Medications Fatigue, arthralgias, myalgias NSAIDs, antimalarials, low-dose prednisone (<10 mg/day). Arthritis NSAIDs, antimalarials, methotrexate Raynaud phenomenon Nifedipine, prazocin Myositis Acute onset/severe - prednisone (60 to 100 mg/day) Myocarditis Trial of steroids and cyclophosphamide Heartburn/dyspepsia H2 antagonists, H+ proton pump blockers, metoclopramide trial Pericarditis NSAID or short course of prednisone Osteoporosis Calcium/vitamin D supplements, bisphosphonates Back to the case • SS showed marked improvement on prednisone • Added – hydroxychlorloquine 200 mg daily – Methotrexte 10 mg weekly – Dimenhydrinate 50-100 mg q6h for N&V • Discharged 8 Oct to community – Plan for 2 weeks prednisone, then Drug Related Problems • SS is experiencing a flare in her MCTD due to lack of suppressive therapy • SS is experiencing GI upset as an adverse effect of prednisone treatment • SS is at risk of worsening anxiety due to lowered paroxetine dose • SS is at risk of osteoporosis from recurrent steroid use • SS is at risk of stomatitis or hepatotoxicity as an adverse effect of methotrexate treatment Recommendation • SS required prophylaxis from steroid induced osteoporisis – Calcium Citrate 400 mg TID – Vitamin D 1000 Units daily • Monitor – attempt taper off steroids – If plan continued to 3 months annual use – Bisphosphonates - etidronate(Didrocal) • Monitor adverse effects (esophageal, ONJ Plan/Follow up • Letter to GP – Recommend calcium, vit D – Etidronate if necessary – Discrepancy on paroxetine dose References • Bennet, R., Axford, J., Romain, P., (2011). Prognosis and treatment of mixed connective tissue disease. Up to Date, ecapp0505p.utd.com207.194.133.9-9974F6FC8B-64913.14 accessed 9 Oct 2011. • Papaioannou, A., Morin, S., Cheung, A. M., Atkinson, S., Brown, J. P., Feldman, S., Hanley, D. a, et al. (2010). 2010 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada: summary. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne, 182(17), 1864-73. doi:10.1503/cmaj.100771