Chronic Fatigue Syndrome - ME Positive
advertisement

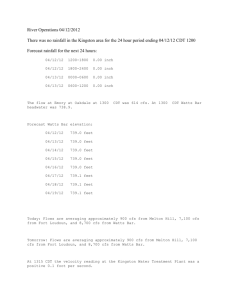
CFS/ME Patient information leaflet Introduction Chronic Fatigue Syndrome/ Myalgic Encephalitis (CFS/ME) is estimated to affect between 50 000 -100 000 people in the UK. It is a diagnosis which is recognised only on clinical grounds and following the exclusion of other conditions. Features include (based on NICE guidance) Fatigue with all of the following features: – New or had a specific onset (that is, it is not life long) – Persistent and/or recurrent – Has resulted in a substantial reduction in activity level characterised by postexertional malaise and/or fatigue (with slow recovery) Including one or more of the following symptoms: – Difficulty with sleeping, such as insomnia, hypersomnia, unrefreshing sleep. – Muscle and/or joint pain that is multi-site and without evidence of inflammation – Headaches or soar throat – Painful lymph nodes without pathological enlargement – Sore throat Cognitive dysfunction – such as difficulty thinking, – inability to concentrate – impairment of short-term memory – difficulties with word-finding – planning/organising thoughts and information processing – Physical or mental exertion makes symptoms worse – General malaise or ‘flu-like’ symptoms – Dizziness and/or nausea – Palpitations in the absence of identified cardiac pathology. The symptoms of CFS/ME fluctuate in severity and may change in nature over time. Symptoms need to have persisted for > 4 months in adults and > 3 months in a child or young person NICE severity scale People with mild CFS/ME are mobile, can care for themselves and can do light domestic tasks with difficulty. Most are still working or in education, but to do this they have probably stopped all leisure and social pursuits, and often take days off. People with moderate CFS/ME have reduced mobility and are restricted in all activities of daily living, although they may have peaks and troughs in their level of symptoms and ability to do activities. They have usually stopped work or education and need rest periods. Their sleep at night is generally poor quality and disturbed. People with severe CFS/ME are unable to do any activity for themselves, or can carry out minimal daily tasks only (such as face washing, cleaning teeth). They have severe cognitive difficulties and depend on a wheelchair for mobility. They are often unable to leave the house, or have a severe and prolonged after-effect if they do so. They may also spend most of their time in bed, and are often extremely sensitive to light and noise. Canadian criteria for diagnosis of CFS/ME Fatigue Post-Exertional Malaise and/or Fatigue: Sleep Dysfunction Pain: joint and muscle aches Headaches Neurological/Cognitive Manifestations: Two or more: Confusion, impairment of concentration and short-term memory consolidation, disorientation, difficulty with information processing, categorizing and word retrieval, perceptual and sensory disturbances. Ataxia, muscle weakness and fasciculations. Overload phenomena: cognitive, sensory – e.g. photophobia and hypersensitivity to noise - and/or emotional overload, which may lead to “crash” periods and/or anxiety. At Least One Symptom from Two of the Following Categories: a. Autonomic Manifestations: orthostatic intolerance - neurally mediated hypotension (NMH), postural orthostatic tachycardia syndrome (POTS), delayed postural hypotension; light-headedness; extreme pallor; nausea and irritable bowel syndrome; urinary frequency and bladder dysfunction; palpitations with or without cardiac arrhythmias; exertional dyspnea. b. Neuroendocrine Manifestations: loss of thermostatic stability – subnormal body temperature and marked diurnal fluctuation, sweating episodes, recurrent feelings of feverishness and cold extremities; intolerance of extremes of heat and cold; marked weight change - anorexia or abnormal appetite; loss of adaptability and worsening of symptoms with stress. Immune Manifestations: tender lymph nodes, recurrent sore throat, recurrent flulike symptoms, general malaise, new sensitivities to food, medications and/or chemicals. The illness persists for at least six months: It usually has a distinct onset, **although it may be gradual. Preliminary diagnosis may be possible earlier. Three months is appropriate for children. To be included, the symptoms must have begun or have been significantly altered after the onset of this illness. It is unlikely that a patient will suffer from all symptoms in criteria 5 & 6. The disturbances tend to form symptom clusters that may fluctuate and change over time. Children often have numerous prominent symptoms varying from day to day. *There is a small number of patients who have no pain or sleep dysfunction, but no other diagnosis fits except ME/CFS. A diagnosis of ME/CFS can be entertained when this group has an infectious illness type onset. **Some patients have been unhealthy for other reasons prior to the onset of ME/ CFS and lack detectable triggers at onset or have more gradual or insidious onset. Investigations Investigations are performed to exclude treatable conditions such as Anaemia, Thyroid abnormalities, Vitamins deficiencies leading to neurological problems Arthritis. Management The aims of treatment are to: Improve activity: sustain or gradually extend, if possible, the person’s physical, emotional and cognitive capacity Manage the physical and impact of their symptoms. Manage the emotional impact of their symptoms Research shows evidence of benefit from cognitive behavioural therapy and/or graded exercise therapy in patients with mild or moderate CFS/ME. Treatment will depend on individual circumstances, duration of condition, symptoms, personal social circumstances. It will therefore be tailored to each individual need*. *(The patient is at liberty to request a cessation of GET/CBT if any negative effects are experienced.") Symptoms such as pain, low mood, sleep disturbance are managed as they would be in standard clinical practice. Apart from medication this can also involve relaxation techniques, advice on sleep management, diet and rest periods. Common mecications used include: amitryptyline, gabapentin, nortryptyline, and zopiclone. NICE recommend that care is supervised/supported by a specialist in CFS/ME. However there is no accredited specialist training to become a specialist. Other specialist services are also involved in management i.e. occupational therapist, physiotherapist and psychologist. Currently the clinical psychology service is severely under resourced. Prognosis A significant proportion of patients do improve and make full recovery, most have some improvement with time. There are some however that may experience setbacks/relapses. Plans can be implemented each person with CFS/ME for managing setbacks/relapses, so that skills, strategies, resources and support are available when needed. Useful contacts George Eliot Hospital CFS/ME clinic Diabetes and Endocrinology Centre George Eliot Hospital NHS Trust, College Street, Nuneaton, CV10 7DJ Ph: 02476351351 Support groups East Midlands ME support group, Tel- 01509 212794 www.mepositive.talktalk.net/ Warwickshire Network for ME Tel - 02476 451526: warksme@yahoo.co.uk Useful web site NICE: www.nice.org.uk Canadian Criteria: www.cfids-cab.org Action for ME: www.afme.org.uk/ The ME Society: www.meassociation.org.uk TYMES Trust : www.youngactiononline.com