GI Physiology V: The Liver and Pancreas
advertisement

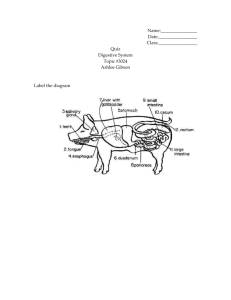
GI Physiology V: The Liver and Pancreas IDP/DPT GI System, Fall 2011 Jerome W. Breslin, Ph.D. LSUHSC-NO Department of Physiology MEB 7208 (1901 Perdido St.) 568-2669 jbresl@lsuhsc.edu Liver & Pancreas Lecture Outline. • Introduction • Exocrine Pancreas • GIP, Glucose, & Insulin Secretion • Pancreatic Juice Composition • Cellular Basis of Secretion • Secretion and Phases of Digestion • Liver • Bile Secretion • Gall Bladder Function Required Reading • Barrett, Gastrointestinal Physiology • Chapter 4 - sections on Pancreas • Chapter 10 - overview and section on enterohepatic circulation • Chapter 11 • Chapter 12 Exocrine Pancreas • Enzymes are produced and secreted in excess. • However, nutrition problems will arise if production of pancreatic enzymes falls by as little as 10%, or if outflow of pancreatic juice is obstructed. Figure 15-25 The exocrine cells in the pancreas play a central role in the production of digestive enzymes; the endocrine functions of the pancreas will be discussed at length in Chapter 16. PANCREATIC JUICE FORMATION Acinar cells secrete proteins into lumen; water & salts follow from blood by a paracellular route. Ductal cells modify secretions of the Acinar cells – add HCO3Acinar Cells Respond to CCK, VIP, GRP & Acetylcholine Na+ K+ Cl- HCO3- Ductule Cells Respond to Secretin & Acetylcholine [HCO3-] increases during elevated pancreatic secretion. pH = 7.2 pH = 8.0 Berne & Levy Fig. 32-19 or Barrett, Fig. 4-4 HCO3 Secretin stimulates secretion in the pancreatic ducts when S cells detect that acid is present in the duodenum. Barrett, Fig. 45 Also see Fig. 4-7 for secretion mechanism Secretin Receptors are Densely Expressed on Pancreatic Ductular Cells in Humans. Stimuli and Second Messengers that mediate elevated secretion by Pancreatic Notes: Acinar Cells Both calcium and cAMP are important, but increasing calcium is more significant than cAMP. Barrett, Fig. 4-7 It is not yet clear whether Secretin modulates secretion from acinar cells in humans, although it does so in rats. Secretin receptors may be present on some subpopulations of acinar cells. INDUCTION OF FLUID SECRETION IN PANCREATIC ACINAR CELLS PANCREATIC SECRETION IN CEPHALIC & GASTRIC PHASES OF DIGESTION PANCREATIC SECRETION IN THE INTESTINAL PHASE Liver: Bile Secretion • Bile is produced in the liver • Bile is stored in the gallbladder. • Bile is secreted into the small intestine. • Bile salts are absorbed in the small intestine and recycled. Figure 15-29 Bile formation by cells in the liver includes 6 components: bile salts, lecithin, bicarbonate ions, cholesterol, bile pigments, and trace metals. The bile is funneled into the gallbladder and then delivered into the duodenum upon stimulation from CCK. Figure 15-31 Cholecystokinin (CCK) stimulates the gallbladder, which responds by contracting and delivering more bile to the duodenum through the sphincter of Oddi, which relaxes (opens) in response to CCK. CCK is secreted by the intestinal mucosa (“I cells”). Bile Acid Structure Primary bile acids are synthesized in the liver. Secondary bile acids are produced in the colon by bacterial enzymes (ursodeoxycholic acid is used as cholesterollowering drug). Figure 15-30 Up to 95% of the cholesterol-based bile salts are “recycled” by reabsorption along the intestine. Formation of cannicular bile in the liver sinusoids: Water Berne & Levy Fig. 32-28 NTCP = Na-dependent taurocholate transporter, OATP = organic ion transport protein, OCT = organic cation transporter, BSEP = bile salt export protein, MDR = multidrug resistance protein, MRP = MDR related protein. Mechanism of bile concentration by gallbladder epithelium Fig. 12-3 Changes in Bile Composition during gallbladder storage Fig. 12-2, Barrett Why? Osmolality is based on the number of particles in solution, whether they be ions, molecules, or micelles. Bile acids form micelles, and essentially the number of particles in solution remains the same because free bile acids incorporate into the micelles as the concentration goes up. Neurohormonal control of gallbladder contraction and biliary secretion. Fig. 12-1 • • • • • Gallstones Estimated that 20 million people in USA have gallstones. Deposition of cholesterol or bilirubin in the gallbladder or in common biliary duct. Cholesterol stones are the common type in Western countries. About 1/3 of patients will get episodes of pain in the epigastric region. Treatment is cholecystectomy (gall bladder removal) or sometimes endoscopic approaches to remove stones from common biliary duct or sphincter of Oddi. Consequence of gall baldder removal is inability to concentrate bile, which affects fat absorption, and Summary • Liver: Bile Production • Enterohepatic circulation - recycling • Gallbladder: Bile Concentration and controls release • CCK is a major regulator Summary of Factors that regulate CCK release: Fig. 4-3 Summary of CCK action on duodenal cluster unit Barrett, Fig. 4-2