eprint_12_12792_1366
advertisement

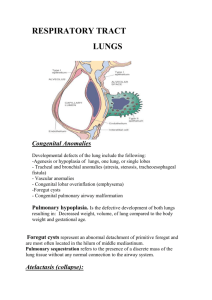
ATELECTASIS (COLLAPSE) Atelectasis, also known as collapse, is loss of lung volume caused by inadeqwate expansion ofairspaces. It results in shunting of inadequately oxygenated blood from pulmonary arteries into veins, thus giving rise to a ventilation-perfusion imbalance and hypoxia. On the basis of the underlying mechanism or the distribution of alveolar collapse, atelectasis is classified into three forms 1-Resorption Atelectasis. Resorption atelectasis occurs when an obstruction prevents air from reaching distal airways. The air already present gradually becomes absorbed, and alveolar collapse follows. Depending on the level of airway obstruction, an entire lung, a complete lobe, or one or more segments may be involved. The most common cause of resorption collapse is obstruction of a bronchus by a mucous or mucopurulent plug. This frequently occurs postoperatively but may also complicate bronchial asthma, bronchiectasis, chronic bronchitis, or the aspiration of foreign bodies, particularly in children. 2- Compression Atelectasis. Compression atelectasis (sometimes called passive or relaxation atelectasis) is usually associated with accumulations of fluid, blood, or air within the pleural cavity, which mechanically collapse the adjacent lung. This is a frequent occurrence with pleural effusions, caused most commonly by congestive heart failure (CHF). Leakage of air into the pleural cavity (pneumothorax) also leads to compression arelectasis 3-Contraction Atelectasis. Contraction (or cicatrization) atelectasis occurs when either local or generalized fibrotic changes in the lung or pleura hamper expansion and increase elastic recoil during expiration. Atelectasis (except that caused by contraction) is potentially reversible and should be treated promptly to prevent hypoxemia and superimposed infection of the collapsed lung 1 Obstructive airway diseases The major diffuse obstructive disorders are emphysema, chronic bronchitis, bronchiectasis, and asthma. Ln patients with these diseases, total lung capacity and forced vital capacity (FVC) are either normal or increased, and the hallmark is a decreased expiratory flow rate, usually measured by forced expiratory volume at 1 second (FEV'). Thus, the ratio of FEVI to FVC is characteristically decreased. Expiratory obstruction may result either from anatomic airway narrowing, classically observed in asthma, or from loss of elastic recoil, characteristic of emphysema Emphysema Emphysema is characterized by abnormal permanent enlargement of the airspaces distal to the terminal bronchioles, accompanied by destruction of their walls without obvious fibrosis Types of Emphysema. Emphysema is classified according to its anatomic distributioa within the lobule; recall that the acinus is the structure distal to terminal bronchioles, and a cluster of three to five acini is called a lobule. There are four major types of emphysema: (1) centriacinar, (2) panacinar, (3) distal acinar, and (4) irregular. Only the first two cause clinically significant airway obstruction, with centriacinar emphysema being about 20-fold more common than panacinar 1-Centriacinar (Centrilobular) Emphysema. The distinctive feature of this type of emphysema is the pattern of involvement of the lobules: the central or proximal parts of the acini, formed by respiratory bronchioles, are affected, while distal alveoli are spared. Thus, both emohvsematous and normal airspaces exist within the same acinus and lobule . The lesions are more common and severe in the upper lobes, particularly in the apical segments. In severe centriacinar emphysema the distal acinus also becomes involved, and so, as noted,the differentiation from panacinar emphysema becomes difficult. This type of emphysema is most commonly seen as a consequence of cigarette smoking in people who do not have congenital deficiency of alpha1-antitrypsin. 2 2- Panacinar (Panlobular) Emphysema. In this type of emphysema, the acini are uniformly enlarged from the level of the respiratory bronchiole to the terminal blind alveoli . In contrast to centriacinar emphysema, panacinar emphysema tends to occur more commonly in the lower lung zones and is the type of emphysema that occurs in u1-antitrypsin deficiency. 3-Distal Acinar (Paraseptal) Emphysema. In this form, the proximal portion of the acinus is normal but the distal part is primarily involved. The emphysema is more striking madjacent to the pleura, along the lobular connective tissue septa, and at the margins of the lobules. It occurs adjacent to areas of fibrosis, scarring, or atelectasis and is usually more severe in the upper half of the lungs. The characteristic findings are the presence of multiple, contiguous, enlarged airspaces that range in diameter from lesst han 0.5mm to more than 2.0cm, sometimesf orming cystlike structures that with progressive enlargement are referred to as bullae. This type of emphysema probably underlies many of the cases of spontaneous pneumothorax in young adults. 4-lrregular Emphysema. Irregular empbysema, so named because the acinus is irregularly inuolued, is almost inuariably associated with scarring, such as resulting from healed inflammatory diseases. Although clinically asymptomatic, this may be the most common form of emphysema. Pathogenesis Current opinion favors emphysema arising as a consequence of two critical imbalances: the protease-antiprotease imbalance and oxidantantioxidant imbalance The protease-antiprotease imbalance hypothesis is based on the observation that patients with a genetic deficiency of the antiproteasea 1antitrypsin have a markedly enhanced tendency to develop pulmonary emphysema, which is compounded by smoking. About 1% of all patients with emphysema have this defect. alpha1-Antitrypsin, normally present in serum, tissue fluids, and macrophages, is a major inhibitor of proteases (particularly elastases) secreted by neutrophils during inflammation. The following sequence is postulated: 1. Neutrophils (the principal source of cellular proteases) are normally sequestered in peripheral capillaries, including those in the lung, and a few gain access to the alveolar spaces. 2. Any stimulus that increases either the number of leukocytes (neutrophils and macrophages) in the lung or the release of their proteasecontaining granules increases proteolytic activity. 3. With low levels of serum alpha 1-antitrypsin, elastic tissue destruction is unchecked and emohysema results. The protease-antiprotease imbalance hypothesis also helps explain the effect of cigarette smoking in the development of emphysema, particularly the centriacinar form in subjects with normal amounts of alpha1-antitrypsin: - ln smokers, neutrophils and macrophages accumulate in alveoli. The mechanism of inflammation is not entirely clear, but possibly involves the direct chemoattractant effects of nicotine as well as the effects of reactive oxygen species contained in smoke. - Accumulated neutrophils are activated and release their granules, rich in a variety of cellular proteases (neutrophil elastase, proteinase 3, and cathepsin G), resulting in tissue damage. - Smoking also enhances elastase activity in macrophages; macrophage elastase is not inhibited by alpha1-antitrypsin and, indeed, can proteolytically digest this antiprotease. Smoking also has a seminal role in perpetuating the oxidant-antioxidant imbalance in the pathogenesis of emphysema. Normally, the lung contains a healthy complement of antioxidants (superoxide dismutase, glutathione) that keep oxidative damage to a minimum Tobacco smoke contains abundant reactive oxygen species (free radicals), which deplete these antioxidant mechanisms,thereby inciting tissue damage Activated neutrophils also add to the pool of reactive oxygen species in the alveoli. A secondary consequence of oxidative injury is inactivation of native antiproteases, resulting in "functional" alpha1-antitrypsin deficiencye ven in patients without enzyme deficiency. Morphology The diagnosisa nd classi f icat ioonf emphysemad ependlargely on the macroscopical appearance of the lung. Panacinar emphysema, when well developed, produces pale, voluminous lungs that often obscure the heart when the anterior chest wall is removed at autopsy. The macroscopic features of centriacinar emphysema are less impressive. The lungs are a deeper pink than in panacinar emphysema and less voluminous,unless the disease is well advanced Generally,i n centriacinar emphysema the upper two- thirds of the lungs is more severely affected than the lower lungs. Histologically there is thinning and destruction of alveolar walls. With advanced disease, adjacent alveoli become confluent creating large airspaces Terminal and respiratory bronchioles may be deformed because of the loss of septa that help tether these structures in the parenchyma. Clinical Course. Dyspnea is usually the first symptom; it begins insidiously but is steadily progressive. In patients with underlying chronic bronchitis or chronic asthmatic bronchitis, cough and wheezing may be initial complaints. Weight loss is common and may be so severe as to suggest a hidden malignant tumor Most individuals with emphysema and COPD fall somewhere between these two classic extremes. In all, secondary pulmonary hypertension develops gradually, arising from both hypoxiainduced pulmonary vascular spasm and loss of pulmonary capillary surface area from alveolar destruction. Death from emphysema is related to either pulmonary failure with respiratory acidosis, hypoxia, and coma, or right-sided heart failure (cor pulmonale). Chronic Bronchitis it is defined as a persistent productiue cougb for at least 3 consecutiue monthsin at least 2 consecutiue years. Pathogenesis. The distinctive feature of chronic bronchitis is hypersecretion of mucus, beginning in the large airways. Although the single most important cause is cigarette smoking, other air pollutants, such as sulfur dioxide and nitrogen dioxide, may contribute. These environmental irritants induce hypertrophy of mucous glands in the trachea and main-stem bronchi and lead to a marked increase in mucin-secreting goblet cells in the surface epithelium of smaller bronchi and bronchioles. In addition, these irritants cause inflammation with infiltration of CD8+ T cells, macrophages, and neutrophils. In contrast to asthma, eosinophils are lacking in chronic bronchitis unless the patient has asthmatic bronchitis. Whereas the defining feature of chronic bronchitis (mucus hypersecretion) is primarily a reflection of large bronchial involvement, the morphologic basis of airflow obstruction in chronic bronchitis is more peripheral and reswhs from (1) so-called "small airway disease," induced by goblet cell metaplasia with mucus plugging of the bronchiolar lumen, inflammation, and bronchiolar wall fibrosis, and (2) coexistent emphysema Microbial infection is often present but has a secondary role, chiefly by maintaining the inflammation and exacerbating symptoms Morphology Grossly, the mucosal lining of the larger airways is usually hyperemic and swollen by edema fluid. lt is often covered by a layer of mucinous or mucopurulent secretions. The smaller bronchi and bronchioles may also be filled with similar secret ions Histologically the diagnostic feature of chronic bronchitis in the trachea and larger bronchi is enlargement of the mucus-secreting glands. The magnitude of the increase in size is assessed by the ratio of the thickness of the submucosal gland layer to that of the bronchial wall (Reid index; normally 0.4). A variable density of inflammatory cells ,largely mononuclear but sometimes admixed with neutrophils, is frequently present in the bronchial mucosa. Clinical Course. In individuals with chronic bronchitis, a prominent cough and the production of sputum may persist indefinitely without ventilatory dysfunction. However, as alluded to earlier, some sufferers develop significant COPD with outflow obstruction. This is accompanied by hypercapnia, hypoxemia, and (in severe cases) cyanosis with progression, chronic bronchitis is complicated by pulmonary hypertension and cardiac failure . Recurrent infections and respiratory failure are constant threats Asthma Asthma is a chronic inflammatory disorder of the airways that causes recurrent episodes of wheezing, breathlessness, chest tightness, and cough, particularly at night and or early in the morning. This clinical picture is caused by repeated immediate hypersensitivity and late-phase reactions in the lung that give rise to the triad of intermittent and reversible airway obstruction, chronic bronchial inflammation with eosinophils, and bronchial smooth muscle cell hypertrophy and hyperreactivity.lt is thought that inflammation causes an increase in airway responsiveness (bronchospasm) to a variety of stimuli. Classification of asthma According to pathophysiological points asthma can be classified into 1- Extrinsic (atopic) asthma: This most common type of asthma usually begins in childhood. A positive family history of atopy is common, and asthmatic attacks are often preceded by allergic rhinitis, urticaria, or eczema.T he diseasei s triggered by environmental antigens, such as dusts, pollen, animal dander, and foods, but potentially any anrigen is implicated. A skin test with the offending antigen results in an immediate wheal-and-flare reaction About 70"/" of cases are said to be "extrinsic" or "atopic" and are due to IgE and TH2-mediated immune responses to environmental antigens. 2-Intrinsic (non atopic) asthma ; In the remaining 30% of patients, asthma is said to be "intrinsic" or "non-atopic" and is triggered by nonimmune stimuli such as aspirin; pulmonary infections, especially those caused by viruses; cold; psychological stress: exercise; and inhaled irritants. Pathogenesis The major etiologic factors of asthma are genetic predisposition to type I hypersensitivity ("atopy"), acute and chronic airway inflammation, and bronchial hyper-responsiveness to a variety of stimuli. The inflammation involves many cell types and numerous inflammatory mediators, but the role of type 2 helper T (T H2) cells may be critical to the pathogenesis of asthma 1- Extrinsic asthma: In the airways there is an initial sensitization to the inhaled inciting antigens, which stimulates induction of Tr12-type cells and release of interleukins IL-4 and IL-5 . This leads to synthesis of IgE that binds to mucosal mast cells. Subsequent IgE mediated reaction to inhaled allergens elicits an immediate response and a late-phase reaction . Exposure of lgE-coated mast cells to the same antigen causes crosslinking of IgE and the release of chemical mediators. Mast cells on the respiratory mucosal surface are initially activated; the resultant mediator release opens mucosal intercellular junctions, allowing penetration of the antigen to more numerous mucosal mast cells. In addition, direct stimulation of subepithelial vagal (parasympathetic) receptors provokes reflex bronchoconstriction through both central and local reflexes. This occurs within minutes after stimulation and is therefore called the acute, or immediate, response, which consists of bronchoconstriction edema (due to increased vascular permeability), and mucus secretion. A variety of inflammatory mediators have been implicated in the acute-phase response, although their relative importance in an actual asthma attack varies widely. Nevertheless, a partial list includes: - Leukotrienes C4, D4, and E4 -Acetylcholine: - Histamine. - Prostaglandin D2 - Platelet-activating factor . Eosinophils are particularly important in the late phase. As mentioned, their accumulation at sites of allergic inflammation is favored by several mast cell-derived chemotactic factors, as well as chemokines (e.g., eotaxin) produced by activated bronchial epithelial cells themselves. The accumulated eosinophils exert a variety of effects. Their armamentarium of mediators is as extensive as that of mast cells and includes major basic protein and eosinophil cationic protein, which are directly toxic to airway epithelial cells. Eosinopbil peroxidase causes tissue damage through oxidative stress. Activated eosinophils are also a rich source of leukotrienes, especially leukotriene C4, which contribute to bronchoconstriction. Thus, eosinophils can amplify and sustain the inflammatory response Morphology The morphologic changes in asthma have been described in persons who die of prolonged severe attacks (status asthmaticus) and in mucosal biopsy specimens of persons challenged with allergens In fatal cases grossly, the lungs are overdistended because of over inflation and there may be small areas of atelectasis. The most striking macroscopic findingis occlusion of bronchi and bronchioles by thick, tenacious mucus plugs. Histologically the mucus plugs contain whorls of shed epithelium (Curschmann spiralsl). Numerous eosinophils and Charcot-Leyden crystals( collections of crystalloids made up of eosinophil proteins) are also present. The other characteristicf indings of asthma, collectively called "airway remodeling" include . Thickening of the basement membrane of th bronchial epithelium. . Edema and an inflammatory infiltrate in the Bronchial walls with a prominence of eosinophils and mast cells. . An increasein the size of the submucosal glands. . Hypertrophy of the bronchial muscle walls. Clinical Course. An attack of asthma is characterized by severe dyspnea with wheezing; the chief difficulty lies in expiration. Bronchiectasis Bronchiectasis is the permanent dilation of bronchi and bronchioles caused by destruction of the muscle and elastic supporting tissue, resulting from or associated with chronic necrotizing infections. It is not a primary disease but rather is secondary to persisting infection or obstruction caused by a variey of conditions The conditions that most commonly predispose to bronchiectasis include the following: - Bronchial obstruction. Common causes are tumors, foreign bodies, and occasionally impaction of mucus. Under these conditions,the bronchiectasis is localized to the obstructed lung segment. Bronchiectasis can also complicate atopic asthma and chronic bronchitis. . Congenital or hereditary conditions. Only a few are cited: In cystic fibrosis, widespread severe bronchiectasis results from obstruction and infection caused by the secretion of abnormally viscid mucus. - In immunodeficiency states, particularly immunoglobulin deficiencies, bronchiectasis is likely to develop because of an increased susceptibility to repeated bacterial infections; localized or diffiuse bronchiectasis can occur. - Kartagener syndrome, an autosomal recessive disorder, is frequently associated with bronchiectasis and with sterility in males. Structural abnormalities of the cilia impair mucociliary clearance in the airways, leading to persistent infections, and reduce the mobility of spermatozoa. Necrotizing, or suppurative, pneumonia, particuIarly with virulent organisms such as Staphylococcus aureus or Klebsiella spp., may predispose to bronchiectasis. In the past, postinfective bronchiectasis was sometimes a sequel to the childhood pneumonias that complicated measles, whooping cough, and influenza, but this has substantially decreased with the advent of successful immunization. Post-tubercular bronchiectasis continues to be a significant cause of morbidity in endemic areas. Pathogenesis. Two processes are crucial and intertwined in the pathogenesis of bronchiectasis: obstruction and chronic persistent infection. Either of these two processes may come first. Normal clearance mechanisms are hampered by obstruction, so secondary infection soon follows; conversely, chronic infection in time causes damage to bronchial walls, leading to weakening and dilation. For example, obstruction caused by a bronchogenic carcinoma or a foreign body impairs clearance of secretions, providing a fertile soil for superimposed infection. The resultant inflammatory damage to the bronchial wall and the accumulating exudate further distend the airways, leading to irreversible dilation. Conversely, a persistent necrotizing inflammation in the bronchi or bronchioles may cause obstructive secretions, inflammation throughout the wall (with peribronchial fibrosis and traction on the walls), Morpbology Bronchiectatic involvement of the lungs usually affects the lower lobes bilaterally, particularly those air passages that are most vertical When tumors or aspiration of foreign bodies lead to bronchiectasis, involvement may be sharply localized to a single segment of the lungs. Usually the most severe involvements found in the more distal bronchi and bronchioles The airways may be dilated to as much as four times their usual diameter and on gross examination of the lung can be followed almost to the pleural surfaces . By contrast ,in normal lungs, the bronchioles can not be followed by ordinary gross examination beyond a point 2-3cm from the pleural surfaces.) The histologicf indings vary with the activity and chronicity of the disease. In the full-blown active case, an intense acute and chronic inflammatory exudate within the walls of the bronchi and bronchioles and the desquamation of lining epithelium cause extensive areas of ulceration. In the usual case a mixed flora can be cultured from the involved bronchi, including staphylococci, streptococci, pneumococci, enteric organisms, anaerobic and microaerophilic bacteria and (particularly in children) Haemophilus influenzae and Pseudomonas aeruginosa. When healing occurs the lining epithelium may regenerate completely; however, usually so much injury has occurred that abnormal dilation and scarring persist. Fibrosis of bronchial and bronchiolar walls and peri bronchiolar fibrosis develop in more chronic cases