TYPICAL DISORDERS OF RESPIRATORY DYSFUNCTION
TYPICAL DISORDERS OF RESPIRATORY DYSFUNCTION.
I.
Disturbances in alveolar ventilation: alveolar hyper- and hypoventilation.
II.
Disturbances in pulmonary circulation.
III.
Abnormal gas exchange through alveolar-capillary barrier.
IV.
Improper matching of ventilation and perfusion.
These and other disturbances underlie the development of respiratory insufficiency (see the scheme above).
Alveolar hyperventilation exists when PaCO
2
is below 37 mm Hg. Hypoxemia controls ventilation by stimulating the peripheral chemoreceptors. In pulmonary disorders and congestive heart failure, hyperventilation results from stimulation of afferent vagal receptors in the lungs and airways. Low cardiac output and hypotension stimulate the peripheral chemoreceptors and inhibit the baroreceptors, both of which increase ventilation. Metabolic acidosis that occurs in many conditions activates both the peripheral and central chemoreceptors. Psychogenic states and severe cerebrovascular insufficiency may interfere with the inhibitory influence normally exerted by cortical structures of the brainstem respiratory neurons. Fever and sepsis also cause hyperventilation through the effects on midbrain and hypothalamus.
The alkalemia associated with hypocapnia may produce dizziness, visual impairment, syncope and seizure which are secondary to cerebral vasoconstriction. Tetany is secondary to decreased free serum calcium and muscle weakness is secondary to hypophosphatemia. Patients with a primary respiratory alkalosis are also prone to periodic breathing and central sleep apnea.
Alveolar hypoventilation is clinically important when PaCO
2
is generally in the range of 50 to
80 mm Hg.
Mechanisms of alveolar hypoventilation:
I. Disturbances of respiratory mechanics: a) obstructive disorders and b) restrictive disorders
(parenchymal and extraparenchymal)
II. Dysfunction of respiratory control: a) abnormalities in peripheral and central chemoreceptors and b) impaired function of brainstem respiratory neurons
Obstructive hypoventilation is characterized by an increase in resistance to airflow owing to partial or complete obstruction at any level, from trachea to respiratory bronchioles. The major obstructive disorders are emphysema, chronic bronchitis, bronchiectasis and asthma as well as a compression or obturation of airways. Any process that narrows the airway lumen leads to early airway closure. Patients must increase their resistance work in order to overcome increased airways resistance forces. In this condition, the interpleural pressure may become positive leading to airway compression and further increasing airway resistance. Excess mucus production and contraction of bronchial smooth muscle, as occurs in asthma and chronic bronchitis, or loss of radial traction on the airways due to destruction of alveolar septa, as occurs in emphysema, are most common causes of early airway closure.
In obstructive diseases, the total lung capacity is normal or increased. The hallmark of an obstructive disorder is a decrease in the forced expiratory volume in one second (FEV
1
) and a reduction of the ratio of FEV
1
to forced vital capacity.
Restrictive hypoventilation is characterized by reduced expansion of lung parenchyma with decreased total lung capacity. Most common parenchymal restrictive disorders are sarcoidosis, idiopathic pulmonary fibrosis, pneumoconiosis and drug- or radiation-induced interstitial lung diseases. Adult respiratory distress syndrome illustrates an example of acute restrictive disease.
Extraparenchymal restrictive disorders include neuromuscular disorders and chest wall disorders.
Most common neuromuscular disorders are poliomyelitis, peripheral neuropathy, myasthenia gravis, muscular dystrophies and high cervical trauma whereas chest wall disorders include obesity, pleural diseases, kyphoscoliosis and ankylosing spondylitis.
The hallmark of a restrictive pattern, found in either parenchymal and extraparenchymal restrictive disorders, is a decrease in lung volumes, primary total lung capacity and vital capacity.
Dysfunction of respiratory control may result from abnormalities in peripheral and central chemoreceptors as well as brainstem respiratory neurons. Defect of peripheral and central
chemoreceptors may be observed in carotid body dysfunction, prolonged hypoxia and metabolic acidosis. Impaired function of brainstem respiratory neurons occurs in bulbar poliomyelitis, encephalitis, brainstem infarction and primary alveolar hypoventilation syndrome.
DISORDERS OF PULMONARY CIRCULATION.
All diseases of the respiratory system causing hypoxemia are potentially capable of increasing pulmonary vascular resistance, since alveolar hypoxia is a very potent stimulus for pulmonary vasoconstriction. Pulmonary vascular resistance increases if intraluminal thrombi or proliferation of smooth muscle in vessel walls diminishes the luminal cross-sectional area. Disturbances in the pulmonary vasculature may result from primary cardiac disease or conditions that elevate left atrial pressure, such as mitral stenosis.
DISTURBANCES OF THE LUNGS DIFFUSION CAPACITY.
Pulmonary diseases may affect the process of diffusion of O2 and CO2 by reducing the exchange surface area or increasing the diffusion distance. The former may occur in emphysema, which destroys the alveolar septa and the latter is observed in interstitial lung disease and pulmonary edema. Under normal circumstances, the diffusion is rapid, and equilibrium of both gases is complete within one-third of the transit time of erythrocytes through the pulmonary capillary bed. Consequently, in patients diffusion abnormality rarely results in arterial hypoxemia at rest. If erythrocyte transit time is shortened, as occurs with exercise, then diffusion limitation may contribute to hypoxemia.
DISTURBANCES OF VENTILATION-PERFUSION MATCHING.
Gas exchange depends critically on the proper matching of ventilation and perfusion at the acinar level. Increased ventilation raises the arterial blood oxygen tension toward the inspired oxygen pressure whereas increased blood flow causes the arterial oxygen tension to decline toward the mixed venous oxygen tension. The most efficient gas exchange occurs when the ventilationperfusion ratio (VPR) is approximately equal to 1. In the presence of pulmonary disease, the VPR can vary from zero to infinity.
A low VPR occurs in physiologic and anatomic shunts. When blood from areas with low ventilated mixes with blood from well-ventilated areas, the resultant mixture has an oxygen content dependent on the oxygen tension in the two areas as well as the relative amounts of blood flow from each. An anatomic shunt may be intra- or extrapulmonary. Extrapulmonary anatomic shunts may result from congenital cardiac malformation. Shunting of blood through the pulmonary parenchyma occurs if the alveoli are atelectatic or if they are filled with fluid.
A high VPR is caused either by excessive ventilation or inadequate blood flow to an area of the lung. A high VPR does not cause arterial hypoxia per se. However, if the overall ventilation is normal, excessive ventilation in one section of the lung means there is inadequate ventilation in others. In areas of the lung where the VPR exceeds 1, the alveolar and capillary oxygen tensions are high but the oxygen uptake is poor. Because of the plateau of the oxygen-hemoglobin dissociation curve, oxygen exchange is inefficient because very little extra oxygen is added to the blood by excess ventilation.
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
Chronic obstructive pulmonary disease (COPD) or chronic obstructive airways disease
(COAD) are commonly-used clinical terms for a group of pathological conditions in which there is chronic, partial or complete, obstruction to the airflow at any level from trachea to the smallest airways resulting in functional disability of the lungs. The obstructive pulmonary disease must be distinguished from restrictive pulmonary disease. The following 4 entities are included in COPD:
1.
Chronic bronchitis
2.
Emphysema
3.
Bronchial asthma
4.
Bronchiectasis
Chronic bronchitis and emphysema are quite common and often occur together. More recently, small airways disease involving inflammation of small bronchi and bronchioles (bronchiolitis) has been added to the group of COPD.
1. CHRONIC BRONCHITIS
Chronic bronchitis is a common condition defined clinically as persistent cough with expectoration on most days for at least three months of the year for two or more consecutive years.
The cough is caused by oversecretion of mucus. In spite of its name, chronic inflammation of the bronchi is not a prominent feature. The condition is more common in middle-aged males than females; approximately 20% of adult men and 5% of adult women have chronic bronchitis, but only a minority of them develop serious disabling COPD or cor pulmonale. Quite frequently, chronic bronchitis is associated with emphysema.
ETIOPATHOGENESIS.
The two most important etiologic factors responsible for majority of cases of chronic bronchitis are: cigarette smoking and atmospheric pollution. Other contributory factors are occupation, infection, familial and genetic factors.
1. Smoking . The most commonly identified factor implicated in causation of chronic bronchitis and in emphysema is heavy smoking. Heavy cigarette smokers have 4 to 10 times higher proneness to develop chronic bronchitis. Prolonged cigarette smoking appears to act on the lungs in a number of ways: a) It impairs ciliary movement, b) It inhibits the function of alveolar macrophages. c) It leads to hypertrophy and hyperplasia of mucus-secreting glands. d) It causes considerable obstruction of small airways. e) It stimulates the vagus and causes broncho-constriction.
2. Atmospheric pollution.
The incidence of chronic bronchitis is higher in industrialized urban areas where air is polluted. Some of the atmospheric pollutants which increase the risk of developing chronic bronchitis are sulfurdioxide, nitrogen dioxide, particulate dust and toxic fumes.
3. Occupation.
Workers engaged in certain occupations such as in cotton mills (byssinosis), plastic factories etc are exposed to various organic or inorganic dusts which contribute to disabling chronic bronchitis in such individuals.
4. Infection.
Bacterial, viral and mycoplasmal infections donot initiate chronic bronchitis but usually occur secondary to bronchitis. Cigarette smoke, however, predisposes to infection responsible for acute exacerbation in chronic bronchitis.
5. Familial and genetic factors.
There appears to be a poorly-defined familial tendency and genetic predisposition to develop disabling chronic bronchitis. However, it is more likely that nonsmoker family members who remain in the air-pollution of home are significantly exposed to smoke
(passive smoking) and hence have increased blood levels of carbon monoxide.
PATHOLOGIC CHANGES.
Grossly, the bronchial wall is thickened, hyperaemic and oedematous. Lumina of the bronchi and bronchioles may contain mucus plugs and purulent exudate.
Microscopically, the characteristic features are as follows:
1.
The cartilage-containing large airways have hypertrophy and hyperplasia of submucosal mucous glands. The increase in thickness can be quantitatively assessed by Reid index which is the ratio between thickness of the submucosal glands to that of the bronchial wall. The bronchial epithelium may show squamous metaplasia and dysplasia.
2.
The non-cartilage containing small air ways show goblet cell hyperplasia and intraluminal and peribronchial fibrosis.
CLINICAL FEATURES.
There is considerable overlap of clinical features of chronic bronchitis and pulmonary emphysema (described later) as quite often the two coexist.
2. EMPHYSEMA
The WHO has defined pulmonary emphysema as combination of permanent dilatation of air spaces distal to the terminal bronchioles and the destruction of the walls of dilated air spaces. Thus,
emphysema is defined morphologically, while chronic bronchitis is defined clinically. Since the two conditions coexist frequently and show considerable overlap in their clinical features, it is usual to label patients as 'predominant emphysema' and 'predominant bronchitis'.
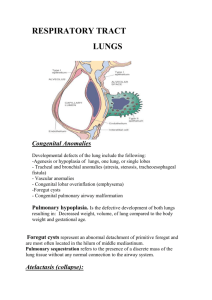
CLASSIFICATION . As mentioned in the beginning of this chapter, a lobule is composed of about 5 acini distal to a terminal bronchiole and that an acinus consists of 3 to 5 generations of respiratory bronchioles and a variable number of alveolar ducts and alveolar sacs. By strictly adhering to the WHO definition of pulmonary emphysema, it is classified, according to the portion of the acinus involved, into 5 types: centriacinar, panacinar (panlobular), para-septal (distal acinar), irregular (para-cicatricial) and mixed (unclassified) emphysema. A number of other conditions to which the term 'emphysema' is losely applied are, in fact, examples of ‘overinflation’. The morphologic appearance of the individual types is described later.
Classification of 'True Emphysema' and 'Overinflation'.
A. TRUE EMPHYSEMA
1.
Centriacinar (centrilobular) emphysema
2.
Panacinar (panlobular) emphysema
3.
Paraseptal (distal acinar) emphysema
4.
Irregular (para-cicatricial) emphysema
5.
Mixed (unclassified) emphysema
B. OVERINFLATION
1.
Compensatory overinflation (compensatory emphysema)
2.
Senile hyperinflation (aging lung, senile emphysema)
3.
Obstructive overinflation (infantile lobar emphysema)
4.
Unilateral translucent lung (unilateral emphysema)
5.
Interstitial emphysema (surgical emphysema) 'overinflation'.
ETIOLOGY AND PATHOGENESIS.
The commonest form of COPD is the combination of chronic bronchitis and pulmonary emphysema. Chronic bronchitis, however, doesnot always lead to emphysema nor all cases of emphysema have changes of chronic bronchitis. The association of the two conditions is principally linked to the common etiologic factors; most importantly, tobacco smoke and air pollutants. Other less significant contributory factors are occupational exposure, infection and somewhat poorly-understood familial and genetic influences. All these factors have already been discussed above.
However, the pathogenesis of the most significant event in emphysema, the destruction of the alveolar walls, is not linked to bronchial changes but is closely related to deficiency of serum alpha-
1-antitrypsin (ccl-protease inhibitor) commonly termed protease-antiprotease hypothesis detailed below.
Protease-antiprotease hypothesis. Alpha-1-anti-trypsin, also called ocl-protease inhibitor, is a glycoprotein that forms the normal constituent of the otl-globulin fraction of the plasma proteins on serum electrophoresis. The single gene locus that codes for cc-1-antitrypsin is located on the long arm of chromosome 14 that codes for immunoglobulin light chains as well. It is normally synthesised in the liver and is distributed in the circulating blood, tissue fluids and macrophages.
The normal function of al-antitrypsin is to inhibit proteases and hence its name ocl-protease inhibitor. The proteases (mainly elastases) are derived from neutrophils. Neutrophil elastase has the capability of digesting lung parenchyma but is inhibited from doing so by anti-elastase (i.e. by alantitrypsin).
Deficiency of the enzyme al-antitrypsin develops in homozygous state due to genetically abnormal locus for protease inhibitor (Pi). The normal phenotype of individuals in homo-zygote is called PiMM, while the most common abnormal phenotype in classic al-antitrypsin deficiency in homozygous state is PiZZ. The heterozygote pattern of PiMZ is not sufficient to produce clinical
deficiency, but heterozygote individuals who smoke heavily have higher risk of developing emphysema.
The a-l-antitrypsin deficiency develops in adults and causes pulmonary emphysema in smokers as well as in non-smokers, though the smokers become symptomatic about 15 years earlier than non-smokers. The other organ showing effects of al-antitrypsin deficiency is liver which may develop obstructive jaundice early in infancy, and cirrhosis and hepatoma late in adulthood.
The mechanism of alveolar wall destruction in emphysema by elastolytic action is based on the imbalance between proteases (chiefly elastase) and anti-proteases (chiefly anti-elastase)':
By decreased anti-elastase activity i.e. deficiency of a-1-antitrypsin.
By increased activity of elastase i.e. increased neutrophilic infiltration in the lungs causing excessive elaboration of neutrophil elastase.
There are enough evidences to suggest that smoking promotes emphysema by both decreasing the amount of anti-elastase as well as by increasing the elastolytic protease in the lungs. These are as under:
1. Oxidant in cigarette smoke has inhibitory influence on a-1-antitrypsin thus lowering the level of anti-elastase activity.
2. Smokers have upto ten times more phagocytes and neutrophils in their lungs than non smokers.
Thus they have very high elastase activity.
PATHOLOGIC CHANGES.
Emphysema can be diagnosed with certainty only by gross and histologic examination of sections of whole lung. The lungs should be perfused with formalin under pressure in inflated state to grade the severity of emphysema with naked eye.
Grossly, the lungs are voluminous, pale with little blood. The edges of the lungs are rounded.
Mild cases show dilatation of air spaces visible with hand lens. Advanced cases show subpleural bullae and blebs bulging outwards from the surface of the lungs with rib markings between them.
The bullae are air-filled cyst-like or bubble-like structures, larger than 1 cm in diameter. They are formed by the rupture of adjacent air spaces while blebs are the result of rupture of alveoli directly into the subpleural interstitial tissue and are the common cause of spontaneous pneumo-thorax.
Microscopically, depending upon the type of emphysema, there is dilatation of air spaces and destruction of septal walls of part of acinus involved i.e. respiratory bronchioles, alveolar ducts and alveolar sacs. Changes of bronchitis may be present. Bullae and blebs when present show fibrosis and chronic inflammation of the walls.
CLINICAL FEATURES.
Cases of 'predominant emphysema' develop clinical features after about one third of the pulmonary parenchyma is damaged which occurs most severely in panacinar emphysema. The age at the time of diagnosis is often a decade later (about 60 years) than the age for predominant bronchitis (about 50 years). Though there is considerable overlap between the clinical features of chronic bronchitis and emphysema, the following features generally characterise
'predominant emphysema':
1.
There is long history of slowly increasing severe exertional dyspnoea.
2.
Patient is quite distressed with obvious use of accessory muscles of respiration.
3.
Chest is barrel-shaped and hyper-resonant.
4.
Cough occurs late after dyspnoea starts and is associated with scanty mucoid sputum.
5.
Recurrent respiratory infections are not frequent.
6.
Patients are called 'pink puffers' as they remain well oxygenated and have tachypnoea.
7.
Weight loss is common.
8.
Features of right heart failure (cor pulmonale) and hypercapneic respiratory failure are the usual terminal events.
9.
Chest X-ray shows small heart with hyperinflated lungs.
3. BRONCHIAL ASTHMA
Asthma is a disease of airways that is characterised by increased responsiveness of the tracheobronchial tree to a variety of stimuli resulting in widespread spasmodic narrowing of the air passages which may be relieved spontaneously or by therapy. Asthma is an episodic disease
manifested clinically by paroxysms of dyspnoea, cough and wheezing. However, a severe and unremitting form of the disease termed status asthmaticus may prove fatal.
Bronchial asthma is common and prevalent worldwide. It occurs at all ages but nearly 50% of cases develop it before the age of 10 years. In adults, both sexes are affected equally but in children there is 2 : 1 male-female ratio.
ETIOLOGY AND PATHOGENESIS AND TYPES.
Based on the stimuli initiating bronchial asthma, two broad etiologic types are traditionally described: extrinsic (allergic, atopic) and intrinsic (idiosyncratic, non-atopic) asthma. A third type is a mixed pattern in which the features donot fit clearly into either of the two main types.
1. Extrinsic (atopic, allergic) asthma. This is the most common type of asthma. It usually begins in childhood or in early adult life. Most patients of this type of asthma have personal and/or family history of preceding allergic diseases such as rhinitis, urticaria or infantile eczema.
Hypersensitivity to various extrinsic antigenic substances or 'allergens' is usually present in these cases. Most of these allergens cause ill-effects by inhalation e.g. house dust, pollens, animal danders, moulds etc. Occupational asthma stimulated by fumes, gases and organic and chemical dusts is a variant of extrinsic astnma. inere are increased levels of IgE in the serum and positive skin test with the specific offending inhaled antigen representing an IgE-mediated type I hypersensitivity reaction which includes an 'acute immediate response' and a 'late phase reaction'.
The acute immediate response is initiated by IgE-sensitised mast cells (tissue counterparts of circulating basophils) on the mucosal surface. Mast cells on degranulation release mediators like histamine, leukotrienes, prostaglandins, platelet activating factor and chemotactic factors for eosinophils and neutrophils. The net effects of these mediators are bronchoconstriction, oedema, mucus hypersecretion and accumulation of eosinophils and neutrophils.
The late phase reaction follows the acute immediate response and is responsible for the prolonged manifestations of asthma. It is caused by 'excessive mobilisation of blood leucocytes that include basophils besides eosinophils and neutrophils. These result in further release of mediators which accentuate the above-mentioned effects. In addition, inflammatory injury is caused by neutrophils and by major basic protein (MBP) of eosinophils.
2. Intrinsic (idiosyncratic, non-atopic) asthma. This type of asthma develops later in adult life with negative personal or family history of allergy, negative skin test and normal serum levels of
IgE. Most of these patients develop typical symptom-complex after an upper respiratory tract infection by viruses. Associated nasal polypi and chronic bronchitis are commonly present. There are no recognisable allergens but abut 10% of patients become hypersensitive to drugs, most notably to small doses of aspirin (aspirin-sensitive asthma).
3. Mixed type. Many patients donot clearly fit into either of the above two categories and have mixed features of both. Those patients who develop asthma in early life have strong allergic component, while those who develop the disease late tend to be non-allergic. Either type of asthma can be precipitated by cold, exercise and emotional stress.
Contrasting Features of the Two Major Types of Asthma.
Feature Exrinsic asthma Intrinsic asthma
1
2
3
Age at onset
Personal/family history
Preceding allergic illness (atopy)
In childhood
Commonly present
Present (e.g. rhinitis, urticaria, eczema)
In adult
Absent
Absent
4 Allergens
Present (dust, pollens, danders etc)
None
5
6
8
Drug hypersensitivity
Serum IgE levels
7 Associated chronic bronchitis, nasal polyps
Emphysema
None
Elevated
Absent
Unusual
Present (usually to aspirin)
Normal
Present
Common
PATHOLOGIC CHANGES.
The pathologic changes are similar in both major types of asthma. The pathologic material examined is generally autopsy of lungs in patients dying of status asthmaticus but the changes are expected to be similar in non-fatal cases. Grossly, the lungs are overdistended due to over-inflation. The cut surface shows characteristic occlusion of the bronchi and bronchioles by viscid mucus plugs. Microscopically, the following changes arc observed:
1.
The mucus plugs contain normal or degenerated respiratory epithelium forming twisted strips called Curschmann's spirals.
2.
The sputum usually contains numerous eosinophils and diamond-shaped crystals derived from eosinophils called Charcot - Leyden crystals.
3.
The bronchial wall shows thickened basement membrane of the bronchial epithelium, submucosal oedema and inflammatory exudate consisting of lymphocytes and plasma cells with prominence of eosinophils. There is hypertrophy of submucosal glands as well as of the bronchial smooth muscle.
4.
Changes of bronchitis and emphysema may supervene, especially in intrinsic asthma.
CLINICAL FEATURES.
Asthmatic patients suffer from episodes of acute exacerbations interspersed with symptom-free periods. Characteristic clinical features are paroxysms of dyspnoea, cough and wheezing. Most attacks typically last for a few minutes to hours. When attacks occur continuously it may result in more serious condition called status asthmaticus. The clinical diagnosis is supported by demonstration of circulation eosinophilia and sputum demonstration of
Curschmann's spirals and Charcot-Leyden crystals. More chronic cases may develop cor pulmonale.
4. BRONCHIECTASIS
Bronchiectasis is defined as abnormal and irreversible dilatation of the bronchi and bronchioles
(greater than 2 mm in diameter) developing secondary to inflammatory weakening of the bronchial walls. The most characteristic clinical manifestation of bronchiectasis is persistent cough with expectoration of copious amounts of foul-smelling, purulent sputum. Post-infectious cases commonly develop in childhood and in early adult life.
ETIOLOGY AND PATHOGENESIS.
The origin of inflammatory destructive process of bronchial walls is nearly always a result of two basic mechanisms: obstruction and infection.
Endobronchial obstruction by foreign body, neoplastic growth or enlarged lymph nodes causes resorption of air distal to the obstruction with consequent atelectasis and retention of secretions.
Infection may be secondary to local obstruction and impaired systemic defense mechanism promoting bacterial growth, or infection may be a primary event i.e. bronchiectasis developing in suppurative necrotising pneumonia.
These 2 mechanisms-endobronchial obstruction and infection, are seen in a number of clinical settings. These are as under:
1. Hereditary and congenital factors.
Several hereditary and congenital factors may result secondarily in diffuse bronchiectasis. These include: a) Congenital bronchiectasis caused by developmental defect of the bronchial system, b) Cystic fibrosis, a generalised defect of exo-crine gland secretions, results in obstruction, infection and bronchiectasis. c) Hereditary immune deficiency diseases are often associated with high incidence of bronchiectasis. d) Immotile cilia syndrome that includes Karta-gener's syndrome (bronchiectasis, situs inver-sus and sinusitis) is characterised by ultrastruc-tural changes in the microtubules causing immotility of cilia of the respiratory tract epithelium, sperms and other cells. Males in this syndrome are often infertile. e) Atopic bronchial asthma patients have often positive family history of allergic diseases and may rarely develop diffuse bronchiectasis.
2. Obstruction.
Post-obstructive bronchiectasis, unlike the congenital-hereditary forms, is of the localised variety, usually confined to one part of the bronchial system. The causes of endobronchial
obstruction include foreign bodies, endobronchial tumours, compression by enlarged hilar lymph nodes and post-inflammatory scarring (e.g. in healed tuberculosis) all of which favour the development of post-obstructive bronchiectasis.
3. As secondary complication.
Necrotising pneumonias such as in staphylococcal suppurative pneumonia and tuberculosis may develop bronchiectasis as a complication.
PATHOLOGIC CHANGES.
The disease characteristically affects distal bronchi and bronchioles beyond the segmental bronchi. Maeroscopically, the lungs may be involved diffusely or segmentally. Bilateral involvement of lower lobes occurs most frequently. More vertical air passages of left lower lobe are more often involved than the right. The pleura is usually fibrotk and thickened with adhesions to the chest wall. Cut surface of the affected lobes, generally the lower zones, shows characteristic honey-combed appearance. The bronchi are extensively dilated nearly to the pleura, their walls are thickened and the lumina are filled with mucus or muco-pus. The intervening lung parenchyma is reduced and fibrotic. The dilated airways, depending upon their gross or bronchographic appearance, have been subclassified into the .following different types: a) Cylindrical: the most common type characterised by tube-like bronchial dilatation. b) Fusiform: having spindle-shaped bronchial dilatation. c) Saccular: having rounded sac-like bronchial distension. d) Varicose: having irregular bronchial enlargements.
Microscopically, fully-developed cases show the following histologic features: a) The bronchial epithelium may be normal, ulcerated or may show squamous metaplasia, b) The bronchial wail shows infiltration by acute and chronic inflammatory cells and destruction of normal muscle and elastic tissue with replacement by fibrosis, c) The intervening lung parenchyma shows fibrosis, while the surrounding lung tissue shows changes of interstitial pneumonia, d) The pleura in the affected area is adherent and shows bands of fibrous tissue between the bronchus and the pleura.
CLINICAL FEATURES.
The clinical manifestations of bronchiectasis typically consist of chronic cough with foul-smelling sputum production, haemoptysis and recurrent pneumonia.
Sinusitis is a common accompaniment of diffuse bronchiectasis. Development of clubbing of the fingers, metastatic abscesses (often to the brain), amyloidosis and cor pulmonale are late complications occurring in cases uncontrolled for years.
CHRONIC RESTRICTIVE PULMONARY DISEASE
The second large group of diffuse lung disease is 'chronic restrictive pulmonary disease' characterised by reduced expansion of lung parenchyma with decreased total lung capacity. This group of diseases must be distinguished from the foregoing COPD. Restrictive lung disease includes 2 types of conditions:
A. Restriction due to chest wall disorder. These causes are:
1) Kyphoscoliosis
2) Poliomyelitis
3) Severe obesity
4) Pleural diseases.
B. Restriction due to interstitial and infiltrative diseases. These are diseases characterized by non-infectious involvement of the interstitial connective tissue of lung parenchyma. The term
'infiltrative' is used here to denote the radiologic appearance of lungs in chest radiographs which show ground-glass shadows due to diffuse infiltration by, small nodules or irregular lines. The conditions included in this group are as under:
I.
Pneumoconiosis
II.
Immunologic lung diseases
III.
Collagen-vascular diseases
IV.
Idiopathic pulmonary fibrosis
V.
Sarcoidosis.
The pathogenesis of the interstitial lung disease is explained by inflammatory reaction causing initial alveolitis in response to various stimuli. In alveolitis, there is accumulation of lymphocytes, macrophages, neutrophils and eosinophils, all of which result in inflammatory destruction of the pulmonary parenchyma followed by fibrosis. Eventually, there is widespread destruction of alveolar capillary walls resulting in end-stage lung or 'honeycomblung'.
The major clinical manifestations of restrictive lung diseases are dyspnoea, tachypnoea and cyanosis, but no wheezing so characteristic of COPD.
After these general comments about the restrictive pulmonary disease, some common and important examples of infiltrative and interstitial lung diseases are described below.
Obstructive versus Restrictive Pulmonary Diseases.
Feature Obstructive Restrictive
1. Airways
2. Pulmonary function test
3. X-ray chest
Obstructed at any level from trachea to respiratory bronchiole
Increased pulmonary resistance and obstruction of maximal expiratory airflow
Variable appearance depending upon the cause
Reduced expansion of lung parenchyma
Decreased total lung capacity
Typically bilateral infiltrates giving ground-glass shadows
Chronic bronchitis
Emphysema
Chest cage disorders (e.g. kyphoscoliosis, poliomyelitis, severe obesity and pleural diseases)
4. Examples
Bronchial asthma
Bronchiectasis
Interstitial and infiltrative diseases (e.g. pneumoconioses, idiopathic pulmonary fibrosis, immunologic lung diseases, collagen-vascular disease and sarcoidosis)