The respiratory system
advertisement
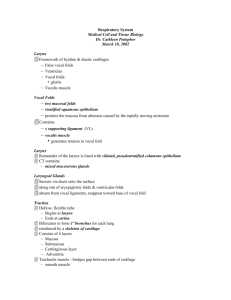
Collage of medicine 9\11\2015 Anatomy and histology department Dr.Hameda A.Gahzi The respiratory system The respiratory system includes the lungs and a series of airways that connect the lungs to the external environment. The respiratory system can be functionally classified into two major subdivisions: 1- a conducting portion, consisting of airways that deliver air to the lungs 2- a respiratory portion, consisting of structures within the lungs in which oxygen in the inspired air is exchanged for carbon dioxide in the blood. This portion of the respiratory system includes the nose, nasopharynx, larynx, trachea, bronchi,and bronchioles of decreasing diameters, including and ending at the terminal bronchioles. These structures warm, moisten, and filter the air before it reaches the respiratory components,where gas exchange occurs. A. Nasal cavity The nares are the nostrils; their outer portions are lined by thin skin, they open into the vestibule, the vestibule is the first portion of the nasal cavity, where the epithelial lining becomes nonkeratinized. Posteriorly, the lining changes to respiratory epithelium (pseudostratified ciliated columnar epithelium with goblet cells). The vestibule contains vibrissae (thick, short hairs), which filter large particles from the inspired air , it has a richly vascularized lamina propria (many venous plexuses) and contains seromucous glands. Olfactory epithelium: The olfactory epithelium is located in the roof of the nasal cavity, on either side of the nasal septum and on the superior nasal conchae. It is a tall, pseudostratified columnar epithelium consisting of olfactory cells, supporting (sustentacular) cells, and basal cells.It has a lamina propria that contains many veins and unmyelinated nerves and houses Bowman glands. 1. Olfactory cells are bipolar nerve cells characterized by a bulbous apical projection (olfactory vesicle) from which several modified cilia extend, olfactory cilia (olfactory hairs) are very long, nonmotile cilia that extend over the surface of the olfactory epithelium , act as receptors for odor. 2. Supporting (sustentacular) cells possess nuclei that are more apically located than those of the other two cell types, have many microvilli and a prominent terminal web of filaments 3. Basal cells rest on the basal lamina but do not extend to the surface, form an incomplete layer of cells are believed to be regenerative for all three cell types. Bowman glands produce a thin, watery secretion that is released onto the olfactory epithelial surface via narrow ducts. Odorous substances dissolved in 1 Collage of medicine 9\11\2015 Anatomy and histology department Dr.Hameda A.Gahzi this watery material are detected by the olfactory cilia. The secretion also flushes the epithelial surface, preparing the receptors to receive new odorous stimuli. B. Nasopharynx The nasopharynx, the posterior continuation of the nasal cavities, becomes continuous with the oropharynx at the level of the soft palate, it is lined by respiratory epithelium, whereas the oropharynx and laryngopharynx are lined by stratified squamous nonkeratinized epithelium. The lamina propria of the nasopharynx, located beneath the respiratory epithelium, contains mucous and serous glands as well as an abundance of lymphoid tissue, including the pharyngeal tonsil. When the pharyngeal tonsil is inflamed, it is called an adenoid. C. Larynx The larynx connects the pharynx with the trachea, the wall of the larynx is supported by hyaline cartilages (thyroid, cricoid, and lower part of arytenoids) and elastic cartilages (epiglottis, corniculate, and tips of arytenoids).The wall also possesses skeletal muscle, connective tissue, and glands. The vocal cords consist of skeletal muscle (the vocalis muscle), the vocal ligament (formed by a band of elastic fibers), and a covering of stratified squamous nonkeratinized epithelium. Contraction of the laryngeal muscles changes the size of the opening between the vocal cords, which affects the pitch of the sounds caused by air passing through the larynx. Inferior to the vocal cords, the lining epithelium changes to respiratory epithelium,which lines air passages down through the trachea and intrapulmonary bronchi. Vestibular folds (false vocal cords) lie superior to the vocal cords. These folds of loose connective tissue contain glands, lymphoid aggregations, and fat cells.They are covered by stratified squamous nonkeratinized epithelium. Trachea and extrapulmonary (primary) bronchi a. The walls of these structures are supported by C-shaped hyaline cartilages (Crings), whose open ends face posteriorly. Smooth muscle (trachealis muscle in the trachea) extends between the open ends of these cartilages. b. Dense fibroelastic connective tissue is located between adjacent C-rings, which permits elongation of the trachea during inhalation. Chapter 15 Respiratory System 231 2. Mucosa 2 Collage of medicine 9\11\2015 Anatomy and histology department Dr.Hameda A.Gahzi a. The respiratory epithelium in the trachea possesses the following cell types. (1) Ciliated cells (a) have long, actively motile cilia that beat toward the mouth. (b) move inhaled particulate matter trapped in mucus toward the oropharynx, thus protecting the delicate lung tissue from damage. (c) also possess microvilli. (2) Mature goblet cells are goblet shaped and are filled with large secretory granules, containing mucinogen droplets, which are secreted onto the epithelial surface to trap inhaled particles. (3) Small mucous granule cells (a) contain varying numbers of small mucous granules. (b) are sometimes called brush cells because of their many uniform microvilli. (c) actively divide and often replace recently desquamated cells. (d) may represent goblet cells after they have secreted their mucinogen. (4) Diffuse neuroendocrine cells (DNES cells) (a) are also known as small granule cells, amine precursor uptake and decarboxylation (APUD) cells, or enteroendocrine cells. (b) contain many small granules concentrated in their basal cytoplasm. (c) synthesize different polypeptide hormones and serotonin. (5) Short (basal) cells (a) rest on the basal lamina but do not extend to the lumen; thus, this epithelium is pseudostratified. (b) are able to divide and replace the other cell types. The basement membrane is a very thick layer underlying the epithelium. The lamina propria is a thin layer of connective tissue that lies beneath the basement membrane. It contains longitudinal elastic fibers separating the lamina propria from the submucosa. The submucosa is a connective tissue layer containing many seromucous glands. The adventitia contains C-shaped hyaline cartilages and forms the outermost layer of the trachea. 3 Collage of medicine 9\11\2015 Anatomy and histology department Dr.Hameda A.Gahzi Intrapulmonary bronchi (secondary bronchi) 1. Intrapulmonary bronchi arise from subdivisions of the primary bronchi. 2. They divide many times and give rise to lobar and segmental bronchi. 3. Their walls contain irregular cartilage plates. 4. They are lined by respiratory epithelium. 5. Spiraling smooth muscle bundles separate the lamina propria from the submucosa, which contains seromucous glands. Primary and terminal bronchioles lack glands in their submucosa. Their walls contain smooth muscle rather than cartilage plates. 4 Collage of medicine 9\11\2015 Anatomy and histology department Dr.Hameda A.Gahzi 1. Primary bronchioles a. Primary bronchioles have a diameter of 1 mm or less. b. They are lined by epithelium that varies from ciliated columnar with goblet cells in the larger airways to ciliated cuboidal with Clara cells in the smaller passages. c. They divide to form several terminal bronchioles after entering the pulmonary lobules. 2. Terminal bronchioles a. Terminal bronchioles are the most distal part of the conducting portion of the respiratory system. b. They have a diameter of less than 0.5 mm. c. They are lined by a simple cuboidal epithelium that contains mostly Clara cells, some ciliated cells, and no goblet cells. d. Function. Clara cells have the following functions: (1) Clara cells divide, and some of them differentiate to form ciliated cells. (2) They secrete glycosaminoglycans. Respiratory portion A. Respiratory bronchioles 1. The respiratory bronchioles mark the transition from the conducting to the respiratory portion of the respiratory system. 2. They are lined by a simple cuboidal epithelium that contains mostly Clara cells and some ciliated cells, except where their walls are interrupted by alveoli, 5 Collage of medicine 9\11\2015 Anatomy and histology department Dr.Hameda A.Gahzi the sites where gas exchange occurs and where the lining abruptly changes to a simple epithelium composed of highly attenuated squamous cells. B. Alveolar ducts 1. Alveolar ducts are linear passageways continuous with the respiratory bronchioles. 2. Their walls consist of adjacent alveoli, which are separated from one another only by an interalveolar septum. 3. They are the most distal portion of the respiratory system to contain smooth muscle cells, which rim the openings of adjacent alveoli and which often appear as knobs in histological sections. 4. Alveolar ducts are lined by type II pneumocytes and the highly attenuated simple squamous epithelium of type I pneumocytes. C. Alveolar sacs are expanded out pouchings of numerous alveoli at the distal ends of alveolar D. Alveoli a. Alveoli are pouch like evaginations about 200 _m in diameter in the walls of respiratory bronchioles, in alveolar ducts, and in alveolar sacs. b. They have thin walls, across which oxygen and carbon dioxide diffuses between the air and the blood. c. They are separated from each other by interalveolar septa that may contain one or more alveolar pores (pores of Kohn). These pores permit equalization of pressure between alveoli. d. They are rimmed by elastic fibers at their openings (except in alveolar ducts, where they are rimmed by smooth muscle cells) and are supported by many reticular fibers in their walls. e. They are lined by a highly attenuated simple squamous epithelium composed of type I and type II pneumocytes. 6 Collage of medicine 9\11\2015 Anatomy and histology department Dr.Hameda A.Gahzi Alveolar cells a. Type I pneumocytes (type I alveolar cells) (1) cover about 95% of the alveolar surface and form part of the blood-gas barrier where exchange of oxygen and carbon dioxide occurs. (2) have an extremely thin cytoplasm that may be less than 80 nm thick (3) form tight junctions with adjacent cells. (4) may have phagocytic capabilities. (5) are not able to divide. b. Type II pneumocytes (type II alveolar cells; great alveolar cells; granular pneumocytes; septal cells) (1) are cuboidal and are most often found near septal intersections. (2) bulge into the alveolus and have a free surface that contains short microvilli around their peripheral borders. (3) are able to divide and regenerate both types of alveolar pneumocytes. (4) form tight junctions with adjacent cells. (5) synthesize pulmonary surfactant, which is stored in cytoplasmic lamellar bodies. Structure—Pulmonary surfactant. Pulmonary surfactant consists of phospholipids and at least four proteins. It forms tubular myelin (a network configuration) when it is first released from lamellar bodies; it then spreads to produce a monomolecular film over the alveolar surface, forming a lower aqueous phase and a superficial lipid phase. 7 Collage of medicine 9\11\2015 Anatomy and histology department Dr.Hameda A.Gahzi (b) Function—Pulmonary surfactant. Pulmonary surfactant reduces the surface tension of the alveolar surface, permitting the alveoli to expand easily during inspiration and preventing alveolar collapse during expiration. Alveolar macrophages (alveolar phagocytes; dust cells) (1) are the principal mononuclear phagocytes of the alveolar surface. (2) remove inhaled dust, bacteria, and other particulate matter trapped in the pulmonary surfactant, thus providing a vital line of defense in the lungs. (3) migrate to the bronchioles after filling with debris. From there, they are carried via ciliary action to the upper airways, eventually reaching the oropharynx, where they are either swallowed or expectorated. (4) may also exit by migrating into the interstitium and leaving via lymphatic vessels. Interalveolar septum The interalveolar septum is the wall, or partition, between two adjacent alveoli. It is bounded on its outer surfaces by the extremely thin simple squamous epithelium lining the alveoli. It contains many elastic and reticular fibers in its thicker regions. It houses continuous capillaries in its central (interior) region.It accommodates the blood-gas barrier, which separates the alveolar airspace from the capillary lumen. 8 Collage of medicine 9\11\2015 Anatomy and histology department 9 Dr.Hameda A.Gahzi