Slow breathing reduces sympathoexitation in patients with
advertisement

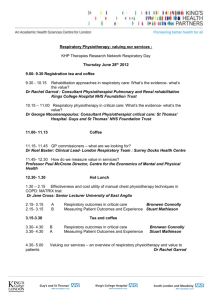
Slow breathing reduces sympathoexcitation in chronic obstructive pulmonary disease Tobias Raupach, MD Florian Bahr Peter Herrmann, PhD Lars Lüthje, MD Karsten Heusser, PhD Gerd Hasenfuß, MD Luciano Bernardi, MD Stefan Andreas, MD Online data supplement Raupach et al.: Slow breathing in COPD First Revision – Manuscript number ERJ-01096-2007 Methods Microneurography Sympathetic nerve activity was measured using microneurographic recordings of efferent muscle sympathetic nerve activity (MSNA) in the peroneal nerve of the right leg. After mapping the course of the peroneal nerve around the head of the fibula by transcutaneous electrical stimulation (Stimuplex HNS 11, B Braun, Melsungen, Germany), a tungsten microelectrode (shaft diameter 200 µm, tip of 1–5 µm) was inserted into the nerve. A reference electrode was inserted subcutaneously 3 cm away. The nerve signals underwent amplification (by 50,000), bandpass filtering (band width 700–2,000 Hz), and passage through a resistance-capacitance integrating network with a time constant of 0.1 second, providing a mean voltage display of sympathetic nerve activity (Nerve Traffic Analysis System, model 662C-3, University of Iowa, Iowa City, USA). The procedure and the criteria for a satisfactory recording of muscle sympathetic nerve activity have been described previously [1, 2]. Sympathetic bursts were identified by inspection of the mean voltage neurogram and quantified as bursts/minute and bursts/100 heartbeats in order to correct for differences in heart rate. Baroreflex sensitivity Baroreflex sensitivity was measured by spectral analysis using the "alpha-angle" method, as previously described [3]. Simultaneous continuous recordings of ECG and blood pressure were sampled at a rate of 256 Hz. Spectral analysis of R-R interval and systolic and diastolic blood pressure was performed after linear detrending by an autoregressive algorithm. Spectral power was calculated as absolute power (variance of the time series), low-frequency (LF) power (0.03-0.15 2 Raupach et al.: Slow breathing in COPD First Revision – Manuscript number ERJ-01096-2007 Hz), and high-frequency (HF) power (0.15-0.4 Hz) [4]. Spontaneous baroreflex sensitivity was estimated as the square root of the relation between LF power of the R-R interval and systolic blood pressure. A mathematical function (squared coherence) was used to prove that fluctuations in the RR interval are in fact related to similar fluctuations in blood pressure [5]. Blood samples A small intravenous catheter was inserted into an antecubital vein before starting the protocol. After a rest of 20 minutes, venous blood samples for catecholamine determinations were drawn into heparinized tubes without applying a tourniquet. The samples were centrifuged immediately and aliquots were stored in screw-top cups at -80° C before carrying out laboratory analyses. Arterial blood gases were measured in an arterial blood sample taken from the radial artery before starting the protocol. Data acquisition and analysis The Modular Intensive Care Data Acquisition System (MIDAS) hardware contains a full programmable 16 channel amplifier and an analog digital converter (ADC) facilitating filtering, amplification and digitalization of biological signals. The ADC delivers full 12-bit accuracy when sampling multiple channels at high gains and fast rates. Several parameters (e.g. gain, sampling rate, and signal range) can be set individually for each channel. The digital signals are first stored in a FIFO (first-infirst-out) buffer and then transferred via USB for further processing. The software for low-level communication between the measuring hardware and the PC was developed with MS Visual C++. The user interface and complete MIDAS software were developed with the graphical programming language G (LabVIEW 6.1, 3 Raupach et al.: Slow breathing in COPD First Revision – Manuscript number ERJ-01096-2007 National Instruments, Austin TX, USA). Communication between this software and MIDAS hardware components is based on a DLL file. The user can select different gains (0.1- to 1000-fold), and sample rates (16 Hz to 8 kHz) for each channel. It is possible to perform a 0-point and 2-point calibration for each signal. The waveform data are stored in a special binary file format. Parts of the raw binary signal can be exported to an ASCII - spreadsheet which can be re-imported to statistics software. 4 Raupach et al.: Slow breathing in COPD First Revision – Manuscript number ERJ-01096-2007 References 1. Delius W, Hagbarth KE, Hongell A, Wallin BG. General characteristics of sympathetic activity in human muscle nerves. Acta Physiol Scand 1972;84:6581. 2. Vallbo AB, Hagbarth KE, Torebjork HE, Wallin BG. Somatosensory, proprioceptive and sympathetic activity in human peripheral nerves. Physiol Rev 1979;59:919-957. 3. Malliani A, Pagani M, Lombardi F, Cerutti S. Cardiovascular neural regulation explored in the frequency domain. Circulation 1991;84:482-92. 4. Keyl C, Schneider A, Gamboa A, Spicuzza L, Casiraghi N, Mori A, Ramirez RT, Leon-Velarde F, Bernardi L. Autonomic cardiovascular function in highaltitude Andean natives with chronic mountain sickness. J Appl Physiol 2003;94:213-9. 5. Bernardi L, Porta C, Spicuzza L, Bellwon J, Spadacini G, Frey AW, Yeung LY, Sanderson JE, Pedretti R, Tramarin R: Slow breathing increases arterial baroreflex sensitivity in patients with chronic heart failure. Circulation 2002;105:143-5 5 Raupach et al.: Slow breathing in COPD First Revision – Manuscript number ERJ-01096-2007 Figure legends Figure S1: Display of continuous tracings of muscle sympathetic nerve activity (MSNA, unprocessed and integrated data), blood pressure and electrocardiogram (ECG) in a healthy control subject. 6 Raupach et al.: Slow breathing in COPD First Revision – Manuscript number ERJ-01096-2007 Tables Table S1. Heart rate during spontaneous, regularized and slow breathing. Heart rate presp pinter 79.0 3.2 COPD Baseline 0.976 patients 79.0 3.1 Respiratory rate 6/min 0.688 69.7 1.7 Healthy Baseline 0.507 controls 70.3 1.9 Respiratory rate 6/min 79.8 3.1 Respiratory rate 15/min COPD 0.193 patients 79.1 3.1 Respiratory rate 6/min 0.629 71.5 1.7 Respiratory rate 15/min Healthy 0.179 controls 70.3 1.9 Respiratory rate 6/min presp, p value for effect of reducing respiratory rate; pinter, p value for effect of interaction between subject group and intervention. Table S2. Systolic and diastolic blood pressure during spontaneous, regularized and slow breathing. Systolic blood pressure presp pinter 127.5 8.2 COPD Baseline 0,219 patients 122.4 6.8 Respiratory rate 6/min 0,388 135.6 7.6 Healthy Baseline 0,698 controls 134.6 7.5 Respiratory rate 6/min 123.7 6.8 COPD Respiratory rate 15/min 0,314 patients 122.4 6.8 Respiratory rate 6/min 0,102 130.7 5.9 Respiratory rate 15/min Healthy 0,163 controls 134.6 7.5 Respiratory rate 6/min Diastolic blood pressure presp pinter 62.8 3.5 COPD Baseline 0,173 patients 64.7 4.0 Respiratory rate 6/min 0,259 68.7 3.4 Healthy Baseline 0,684 controls 68.0 2.7 Respiratory rate 6/min 61.2 3.5 Respiratory rate 15/min COPD 0,053 patients 64.7 4.0 Respiratory rate 6/min 0,479 66.0 2.4 Respiratory rate 15/min Healthy 0,172 controls 68.0 2.7 Respiratory rate 6/min presp, p value for effect of reducing respiratory rate; pinter, p value for effect of interaction between subject group and intervention. 7