Managing elevated blood lead levels: a guide for clinicians
advertisement

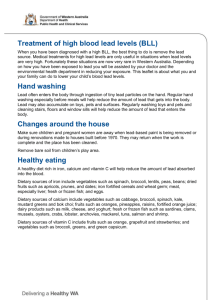
Managing elevated blood lead levels: a guide for clinicians Principles of management Who should be screened for elevated blood levels (BLL)? Please refer to the fact sheet ‘Who should be screened for elevated blood lead levels?’ Confirmation of elevated levels An elevated BLL must be confirmed as the finding of elevated levels might mean considerable disruption to the affected household. The section below on medical management provides more information on when to re-test. Management of acute lead poisoning For management of urgent symptomatic cases please contact the WA Poisons Information Centre 13 11 26 (all hours). Acute lead poisoning with overt symptoms is now rare in Western Australia; most cases identified will be subclinical elevated levels due to chronic exposure picked up on screening. Multi-disciplinary approach The mainstay of managing elevated BLL is identifying and removing the source, reducing lead absorption in an exposed individual, providing information and education to affected individuals and families and careful follow-up to ensure that management is successful. This requires communication between hospitals, the general practitioner, environmental health and the households affected. High risk groups The following groups are particularly vulnerable to the adverse effects of lead and their management should be prioritised; Children (especially those under the age of 5 years) Pregnant women Lactating women In all cases of an elevated BLL (5 µg/dL and above for high-risk groups and 10 µg/dL and above for everyone else): Notify the Executive Director of Public Health (EDPH) within 3 days using the electronic ‘Notification of Lead Poisoning’ notification form or fill out a printed form and fax or post this to the EDPH. Discuss the case with a clinical toxicologist The Environmental Health Directorate is able to provide assistance and information with assessing exposure using the lead exposure questionnaire, carrying out abatement and screening of household contacts. (9388 4999 ask for a toxicologist) 1 Managing elevated blood lead levels: A guide for clinicians continued Provide information to the affected household on reducing exposure and absorption of lead (see the fact sheet ‘Reducing your blood lead levels’). Medical management of elevated BLL For neonates aged less than 1 month, re-test initially within one month. In all cases of an elevated BLL: Remove the exposure or the person from the exposure, whichever is more practicable and provide advice on reducing lead absorption. Repeat blood lead levels six weeks to three months after abatement and then again at six months. Test for iron-deficiency anaemia and manage this accordingly. For a BLL of less than 50 µg/dL, the mainstay of treatment is reducing exposure. A BLL of 50 µg/dL and above is likely to require admission and chelation therapy. Consult with a clinical toxicologist. Elevated BLL in pregnancy Management and re-testing should be carried out in consultation with experts in lead toxicity and high-risk pregnancies. Immediate removal from the lead source is the priority in all cases where BLL is equal to or greater than 5 µg/dL. Elevated BLL and breast-feeding Management and re-testing of mother and child should be carried out in consultation with a paediatrician and a clinical toxicologist. In general, initiation of breast-feeding is encouraged if maternal BLL is less than 40 µg/dL Breast-feeding should continue if the infant’s BLL is less than 5 µg/dL 2