case history 5
advertisement

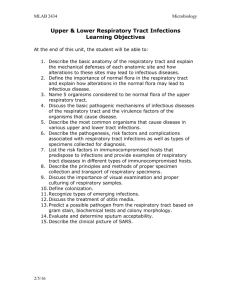
Respiratory Tract Infection Faculty Copy – Page 1 VIROLOGY CASE-BASED SMALL GROUP DISCUSSION SESSION 23 RESPIRATORY TRACT INFECTIONS THURSDAY, MARCH 22, 2001 1:00PM – 3:00PM Reading Assignment: Sherris Medical Microbiology, Chapters 32, 37 Respiratory Tract Infection Faculty Copy – Page 2 CASE HISTORY 1 The patient was a 4-month-old female with congenital heart disease who was admitted to the hospital in January with severe respiratory distress. Five days prior to admission she had developed a cough and rhinitis. Two days later she began wheezing and was noted to have a fever. She was brought to the emergency room when she became lethargic. One sibling was reported to be coughing, and her father had a "cold". On examination she was agitated and coughing. She had a fever of 38.9 0C, tachycardia with a pulse of 220, tachypnea with respirations of 80/min., and a blood pressure of 90/58 mm Hg. Her fontanelles were open, soft, and flat. Her throat was clear. She had subcostal retractions and nasal flaring. On auscultation of her lungs, there were rhonchi as well as inspiratory and expiratory wheezes. A chest radiograph revealed interstitial infiltrates and hyperexpansion. Arterial blood gases on supplemental oxygen revealed respiratory acidosis with relative hypoxemia. She was put in respiratory isolation in the pediatric intensive care unit and was subsequently intubated. Blood and nasopharyngeal cultures were obtained and sent to the bacteriology and virology laboratories. A nasopharyngeal wash specimen was positive for RSV antigen by rapid test and specific antiviral therapy was begun. She was extubated 5 days later and discharged home on day 8. BACKGROUND This patient was found to be infected with RSV (a negative strand RNA virus), which causes severe infections in children less than 1 year old, whereas reinfections in older children and adults may result in minimal respiratory tract symptoms. RSV can also cause acute laryngotracheobronchitis. The elderly may also develop severe RSV infections. The differential diagnosis for this patient's pneumonia includes respiratory viruses such as parainfluenza virus types 1, 2 and 3, influenza A and B viruses, and respiratory syncytial virus (RSV). Bordetella pertussis could also have caused her illness. Respiratory Tract Infection Faculty Copy – Page 3 1. What type of isolation should the patient be put in? Transmission is via contact with respiratory droplets. Because RSV can cause nosocomial infections, patients should be put in contact isolation. If patients are not isolated and infection control practices (strict handwashing, use of gloves and gowns, etc.) are not used, cross-infections can occur at a rate of 20 to 50%. Several patients with RSV can be "cohorted" (put in the same room), and their health care providers can be similarly cohorted. Nosocomial RSV infections are a hazard particularly for other hospitalized patients with congenital heart disease, lung disease, or immunodeficiency states who are at risk for life-threatening RSV infections. Community outbreaks of RSV infection occur annually and can commence at any time from late fall to early spring. The usual outbreak lasts 8 to 12 weeks and can involve nearly one half of all families with children. In the family setting, it appears that older siblings often introduce the virus into the home, and secondary infection rates can be almost 50%. The usual duration of virus shedding is 5 to 7 days; young infants, however, may shed virus for 9 to 20 days or longer. 2. What is known about the pathogenesis of the infection? The virus is spread to the upper respiratory tract by contact with infective secretions. Infections appear to be confined primarily to the respiratory epithelium, with progressive involvement of the middle and lower airways. Viremia occurs rarely. The virus particles are also toxic to tissues. This toxicity can be demonstrated by inoculating high concentrations of inactivated virions into mice, which produces acute inflammatory changes in the absence of viral penetration or replication within cells. The apparent enhanced severity of disease, particularly in very young infants, is not yet clearly understood, but may have an immunologic basis. Factors that have been proposed to play a role include (1) qualitative or quantitative deficits in humoral or secretory antibody responses to critical virus-specified proteins; (2) excessive damage from inflammatory cytokines or direct cell-mediated cytotoxicity; (3) formation of antigen- Respiratory Tract Infection Faculty Copy – Page 4 antibody complexes within the respiratory tract resulting in complement activation; and (4) IgE-mediated histamine release. The usual mortality among infants hospitalized with RSV infections is 0.5 to 1%; however, this rises to 15% or greater in children receiving cancer chemotherapy, infants with congenital heart disease, and those with severe immunodeficiency. Infants with underlying chronic lung disease are also considered to be at high risk for a lethal outcome. Former premies are also high risk-tend to have bronchopulmonary displasia from prolonged ventillation. 3. Describe the rapid test used for detection of RSV. Rapid antigen detection tests are currently available for RSV and influenza A. RSV can be detected in nasopharyngeal washings or aspirates by either an enzyme immunoassay (EIA) or immunofluorescence. Many institutions are replacing immunofluorescence with EIA because EIA is easier to perform, is more rapid when multiple specimens must be tested, and has similar sensitivity and specificity. RSV isolation in cell culture takes 3 to 10 days. The advantage of culture is a higher degree of sensitivity than that of rapid procedures, and culture has the ability to detect a variety of viral agents. However, specimens for RSV culture must be quickly transported and cultured because this virus soon loses infectivity outside the host. Rapid viral antigen tests are valuable because of the length of time required to detect many viruses in culture. Prompt results are preferred so that the decision to use antiviral agents can be made as soon as possible. 4. A formalin fixed-killed virus vaccine was tested against RSV. Why was this vaccine discontinued? This vaccine was discontinued because it predisposed children to more severe disease! 5. Describe the preventative therapy currently in use for selected infants. Palivizumab and RespiGam are currently used to prevent RSV infection in high risk infants. Only one antiviral agent, ribavirin, is available for treatment of RSV in infants. It has been shown to decrease viral shedding and may increase the patient's oxygenation. It is delivered by aerosol to best reach the site of infection and to minimize toxicity. It is generally only given to the highest risk patients because of its extreme cost (>$1000/day). Respiratory Tract Infection Faculty Copy – Page 5 Ribavirin is a nucleoside analogue and is thought to inhibit the viral RNAdependent RNA polymerase. 6. Is this child likely to be reinfected? Yes. Immunity is short-lived and multiple reinfections are possible. However, subsequent disease is generally less severe. Respiratory Tract Infection Faculty Copy – Page 6 CASE HISTORY 2 The patient was a 1-year-old male who was brought to the clinic in January because he developed fever, chest congestion, rhinorrhea, decreased oral intake and a "barking" cough 3 days previously. His medical history was significant only for recurrent otitis media. On examination, his temperature was 38.40C. He was in no acute distress and had audible obstructive upper airway sounds. His throat was erythematous. On lung examination, upper airway sounds were prominent and there was no wheezing or subcostal retractions. The clinical impression was that he had croup. Specimens were sent for viral cultures. He was managed with therapies for symptomatic relief including the use of a humidifier in the home. Ten days later parainfluenza was identified from a nasopharyngeal specimen only after hemadsorption studies were done on the virus culture. BACKGROUND This patient's clinical diagnosis was croup (acute laryngotracheobronchitis). This patient was infected with parainfluenza virus type 1 (PIV-1). PIV is the virus most commonly associated with croup. There are four serotypes of PIV, PIV-1 to PIV-4. Like influenza virus, PIV produces both hemagglutinins and neuraminidase. Unlike influenza virus, PIV has a nonsegmented genome and the four types are antigenically stable. RSV can cause a similar clinical syndrome to PIV. 1. How is the virus transmitted? Transmission is via direct inhalation of particles or contact with contaminated secretions to nasal or conjunctival epithelium. Parainfluenza is a disease seen primarily in children 4 months to 6 years of age. Epidemic disease occurs in the fall with PIV-1 or PIV-2 predominantly in alternate years. PIV-3 appears to be endemic throughout the year. Like all enveloped respiratory viruses, PIV is spread most efficiently by aerosolization. Respiratory Tract Infection Faculty Copy – Page 7 2. What is croup? Why don’t adults get croup? The pathophysiology of croup is due to infection and inflammation in the subglottic area. This leads to a stridorous cough. Manifestations of parainfluenza virus infections are generally more severe in infants and young children than in adults. (adult have a larger subglottic area and therefore the inflammation does not lead to as severe a cough). Infection can result in severe pneumonia, bronchitis, laryngitis, croup (laryngotracheobronchitis), or just a mild upper respiratory tract infection. There are no extrapulmonary manifestations (no viremia). 3. Describe how the clinical diagnosis of croup was confirmed. Is laboratory confirmation critical in all cases? Laboratory confirmation is not critical in cases with “classic” clinical presentation. There is attached a copy of the procedure for working up respiratory specimens. 4. Is this child likely to be re-infected? What is the common symptom in adults with this infections? Yes. Immunity is only transient. Repeat infections, which are usually milder, occur in older children and adults. 5. If this child had more severe croup, what treatment would be appropriate? Recent studies indicate that in children with moderately severe croup, treatment with intramuscular dexamethasone or nebulized budesonide resulted in more rapid clinical improvement than did the administration of placebo, with dexamethasone offering the greatest improvement. Treatment with either glucocorticoid resulted in fewer hospitalization. Respiratory Tract Infection Faculty Copy – Page 8 CASE HISTORY 3 A 16 year-old white female presents with a two week history of sore throat and lethargy. The patient was previously healthy. She had fever to 103 o F. for a few days, and saw her physician, who noted exudate and obtained a throat culture, which was negative for group A streptococcus. Her physician prescribed ampicillin for her symptoms, and after taking several doses, she developed a diffuse macular rash on her trunk and extremities. The question of penicillin allergy arose. She comes to your office because she reports that she still has low grade fever, some sore throat, and feels extremely tired and listless. Physical examination reveals an erythematous pharynx with white exudates on the tonsils, and cervical, axillary, and inguinal adenopathy. Abdominal examination reveals a palpable spleen tip. A blood count reveals a WBC of 12.0 with 20 neutrophils, 5 bands, 30 lymphocytes, 30 atypical lymphocytes which are not blasts, and 15 monocytes. Hemoglobin and platelet count are normal. A monospot test is reported as positive. STUDY QUESTIONS 1. How is the virus transmitted? EBV is transmitted by close contact with respiratory secretions; it is frequently referred to as “the kissing disease.” 2. What is a monospot test and what other laboratory tests may be useful in confirming your preliminary diagnosis? The monospot test detects the presence of heterophile antibody (human serum which will agglutinate sheep red blood cells). This is IgM antibody, and appears during the first or second week of illness, persisting for several months. Many conditions can produce heterophile antibodies, but specific absorption studies allow for specificity of the test for infectious mononucleosis (ie the reaction occurs if the serum is absorbed first with guinea pig kidney antigens, but not if the serum is absorbed first with beef red blood cells-other illnesses will be associated with other absorption patterns). The monospot is an insensitive test in young children. Some false-positive reactions may occur in adolescents and adults. If a more specific test is desired, serum can be tested for IgM and IgG antibodies to EBV viral capsid antigen (VCA). 3. What are the long-term consequences of infection? Respiratory Tract Infection Faculty Copy – Page 9 Most individuals have no long-term consequences following EBV infection. Many infections in normal hosts are asymptomatic. Immunocompromised patients may develop long-term sequelae. Transplant patients may develop an EBV-associated lymphoproliferative disease. Individuals with X-linked lymphoproliferative syndrome cannot mount a normal immune response to EBV, and EBV infection in these individuals may be fatal. Patients with AIDS may develop several EBV-associated disorders: nonHodgkin lymphoma, lymphocytic interstitial pneumonitis, and oral “hairy” leukoplakia. Several malignancies have been associated with EBV infection: Burkitt lymphoma, nasopharyngeal carcinoma, and possibly Hodgkin disease. EBV has not been proved to be associated with “chronic fatigue syndrome.” 4 Are there any effective anti-viral agents that act against this virus? Acyclovir and ganciclovir act on the lytic phase of EBV replication, but not the latent phase, inhibiting EBV DNA polymerase and subsequent viral production. These drugs share no effect on the clinical course of infectious mononucleosis and therefore should not be prescribed for this condition. Acyclovir therapy has been reported to result in regression of oral “hairy” leukoplakia lesions. 5. Is your patient likely to be re-infected? Are family members at risk for infection? What other contacts are likely to be infected? Recurrent infection has not been well-documented, if it occurs at all. Family members are at risk of infection if they share oral secretions. Other individuals who may become infected are the patient’s boyfriend, due to sharing the oral secretions during kissing. 6. Why did the patient have a rash after Ampicillin? Should you tell her that she is allergic to the drug? Ampicillin and other penicillin derivatives frequently are associated with rash when given to patients with infectious mononucleosis. This is a classic association which may provide a clue to the diagnosis. The exact basis for this reaction is unclear, but it is known that it does not represent a hypersensitivity reaction to the drug, which can be safely given to the patient after the infectious mononucleosis illness has resolved. 7. What other pathogens besides EBV can result in an infectious mononucleosis illness? Respiratory Tract Infection Faculty Copy – Page 10 Cytomegalovirus, Toxoplasma gondii, and acute HIV infection can also cause infectious mononucleosis-type illnesses. Also mention Acute EBV hepatitis followed by the appearance of local and humoral antibody along with an evolving, more durable cellular immunity. Finally, there is repair of tissue damage. Respiratory Tract Infection Faculty Copy – Page 11 CASE HISTORY 4 A 75 year-old female residing in a nursing home developed the sudden onset of fever to 101o F, headache and malaise in December. Over the next two days, she had increasing difficulty breathing and was transferred to a medical facility where a diagnosis of pneumonia was made by chest x-ray. Her 2 year old grandson had visited her three days prior to the onset of symptoms. He became ill the day after the visit with cough, rhinorrhea and vomiting. The woman had not received an influenza vaccine that year; her physician deferred the vaccine because the patient had an upper respiratory infection. The woman was treated with antibiotics and oxygen. She gradually recovered. After she was discharged, the clinical virology laboratory isolated influenza B virus from a pharyngeal swab. BACKGROUND Influenza B virus (a negative strand RNA virus with a segmented genome). Influenza viruses have a predilection for the respiratory tract, and viremia is rarely detected. They multiply in ciliated respiratory epithelial cells, leading to functional and structural ciliary abnormalities. This is accompanied by a switchoff of protein and nucleic acid synthesis in the affected cells, the release of lysosomal hydrolytic enzymes, and desquamation of both ciliated and mucusproducing epithelial cells. There is, thus substantial interference with the mechanical clearance mechanism of the respiratory tract. The process of cell death results in the cleavage of complement components, leading to localized inflammation. Early in infection, the primary chemotactic stimulus is directed toward mononuclear leukocytes, which constitute the major cellular inflammatory component. The respiratory epithelium may not be restored to normal for 2 to 10 weeks after the initial insult. The virus particles are also toxic to tissues. This toxicity can be demonstrated by inoculating high concentrations of inactivated virions into mice, which produces acute inflammatory changes in the absence of viral penetration or replication within cells. Other host cells functions are also severely impaired, particularly during the acute phase of infection. They include chemotactic phagocytic, and intracellular killing functions of polymorphonuclear leukocytes and perhaps of alveolar macrophage activity. Respiratory Tract Infection Faculty Copy – Page 12 The net result of these effect, is that on entry into the respiratory tract, the viruses cause cell damage, especially in the respiratory epithelium, which elicits an acute inflammatory response and impairs mechanical and cellular host responses. This damage renders the host highly susceptible to invasive bacterial superinfection. In vitro studies also suggest that bacterial pathogens such as staphylococci can more readily adhere to the surfaces of influenza virus-infected cells. Recovery from infection begins with interferon production, which limits further virus replication, and with rapid generation of natural killer cells. Shortly thereafter, class I major histocompatibility complex (MHC)-restricted cytotoxic T cells appear in large numbers to participate in the lysis of virus-infected cells and, thus, in initial control of the infection. This is followed by the appearance of local and humoral antibody along with an evolving, more durable cellular immunity. Finally, there is repair of tissue damage. 1. How is the virus transmitted? Inhalation or contact with respiratory secretions from an infected person. 2. How is the viral infection detected? During the acute phase of illness, influenza viruses can be readily isolated from respiratory tract specimens, such as nasopharyngeal and throat swabs. Most strains grow in primary monkey kidney cell cultures or in the amniotic cavity of embryonated hen's eggs, and they can be detected by hemadsorption or hemagglutination. Rapid diagnosis of infection is possible by direct immunofluorescence or immunoenzymatic detection of viral antigen in epithelial cells or secretions from the respiratory tract. Serologic diagnosis is of considerable help epidemiologically and is usually made by demonstrating a fourfold or greater increase in complement-fixing or hemagglutination inhibition antibody titers in acute and convalescent specimens collected 10-14 day apart. 3. The woman received a vaccine last year, why wasn’t she still protected? Is a URI a contraindication to vaccination? The best available method of control is by use of killed viral vaccine prepared from those strains related most closely to the antigenic subtypes currently causing infections. (Viral strains change each year due to antigenic drift and shift). These inactivated vaccines may contain whole virions or "split" subunits composed primarily of hemagglutinin antigens. Respiratory Tract Infection Faculty Copy – Page 13 They are commonly used, in two doses given 1 month apart, to immunize children who may not have been immunized previously; otherwise, single annual doses are recommended just prior to influenza season. Used in this way, the virus vaccines may be 70 to 85% effective. It is recommended that vaccination be directed primarily toward the elderly, individuals of all ages who are at high risk (eg, those with chronic lung or heart disease), and their close contacts, including medical personnel and household members. A URI is not contraindication for vaccination. 4. Are there any effective anti-viral agents that act against this virus? Yes. Oseltamivir and zanamivir has been shown to inhibit the replication of influenza A and B strains in vitro, in mice and in experientally induced infection in humans. Hayden et al. report that in a double-bind randomized, placebo-controlled trial conducted over a six-week period during the influenza season, 75 mg of oseltamivir administered once or twice daily (for a total dose of 75 or 150 mg daily) was well tolerated, and its efficacy as prophylaxis against laboratory-documented febrile influenza was 74 percent (95 percent confidence interval, 53 to 88 percent). Once-daily and twice-daily doses provided similar levels of efficacy. Likewise, Monto et al. found that another neuraminidase inhibitor, zanamivir, was approximately 84 percent effective (95 percent confidence interval, 55 to 94 percent) in preventing laboratory-confirmed illness associated with fever. Zanamirvir is an orally inhaled compound that has been approved for influenza treatment in Australia, Europe, and the United States. These specific inhibitors of influenza neuraminidase have been discovered by analyzing the crystallographic structure of this molecule and applying the techniques of rational drug design. These compounds bind to the conserved active site of neuraminidase and appear to inhibit the release of viruses from infected cells and their subsequent spread to adjacent cells. The neuraminidase inhibitors for which data are currently available appear to be effective against both influenza A and influenza B infections. They seem to have less potential than amantadine or rimantadine for inducing resistance and are associated with fewer major side effects, but they are likely to cost more. Amantadine hydrochloride, a symmetric amine, has been shown to be effective in short-term (several weeks) oral prophylaxis of Influenza A INFECTIONS BUT NOT Influenza B. It appears to act by blocking the ion channel of the viral M2 protein, resulting in interference with its key role in Respiratory Tract Infection Faculty Copy – Page 14 early virus uncoating and also later virion assembly. Amantadine can produce side effects, however, and is recommended only for high-risk patient until vaccine-induced immunity can be achieved. A typical example of its use would be during an epidemic in which an elderly, potentially susceptible patient may become exposed to infection within a defined period. Oral amantadine prophylaxis may be initiated concurrently with administration of a vaccine containing the most current continued protection. It must be emphasized that amantadine has been proven effective for influenza A virus infections only; it is useless in other respiratory virus. A newer related drug, rimantadine, seems to be as efficacious as amantadine and may cause fewer adverse effects. Unfortunately, virus resistance to both drugs can develop. A single mutation in the membrane portion of the M2 protein is all that is necessary for this to occur. 5. What recommendation would you suggest for this woman for the next flu season? She should receive the vaccine each year. CASE HISTORY 5 Respiratory Tract Infection Faculty Copy – Page 15 The patient was a 2 ½ year old male, who was admitted to the hospital in August with fever and respiratory distress. Patient was well until one day before when he developed fever, rhinorrhea and congestion. On the day of admission, he was brought to the ER because he seemed to have trouble breathing. His medical history was significant for developmental delay and numerous episodes of aspiration pneumonia. Family history revealed that a 7 year-old sibling and several of his “swim-team” members had pharyngitis and conjunctivitis 10 days ago. On examination, the child’s temperature was 40.80C. He was tachypnic with a respiratory rate of 40. The heart rate was 160. He had moderate mucoid nasal discharge. He had subcostal retractions and nasal flaring. His throat was red and there was exudate on both tonsils. On auscultation of his lungs, there were scattered rhonchi, but no wheezes noted. A chest radiograph revealed no new findings. He was put in respiratory isolation in the pediatric wards. Blood and nasopharyngeal cultures were sent to the microbiology laboratory. A nasopharyngeal wash specimen was positive for adenovirus (was detected by shell vial technique at 480 and confirmed by staining with monoclonal antibodies). BACKGROUND Etiology: Adenoviruses are DNA viruses; at least 51 distinct serotypes divided into 6 subgenera (A to F) cause human infections. Human adenovirus infections are ubiquitous. Adenoviruses are most important clinically because of their capacity to cause acute infections of the respiratory system and conjunctivae. Adenoviruses cause 5-8% of acute respiratory disease in infants and children including pneumonia. The serotype of adenovirus that causes infection and the type of disease induced is closely related to the age of the patient. (See following table) The incidence of adenovirus-induced respiratory tract disease is increased slightly in late winter, spring, and early summer. Enteric disease occurs during most of the year and primarily affects children younger than 4 years of age. Adenovirus infections are most communicable during the first few days of an acute illness, but persistent and intermittent shedding for longer periods, even months, is frequent. The incubation period for respiratory tract infection varies from 2 to 14 days; for gastroenteritis, it is 3 to 10 days. Diseases Caused by Adenoviruses Group Affected Neonates Infants Children Young children Adults Immunocompromised Respiratory Tract Infection Faculty Copy – Page 16 Syndromes Common Causal Adenovirus Serotypes Fatal disseminated infection 3, 7, 21, 30 Coryza, pharyngitis (most 1, 2, 5 asymptomatic) Upper respiratory disease 1, 2, 4-6 Pharyngoconjunctival fever 3, 7 Hemorrhagic cystitis 11, 21 Diarrhea 2, 3, 5, 40, 4 1 Intussusception 1, 2, 4, 5 Meningoencephalitis 2, 6, 7, 12 Acute respiratory disease and 3, 4, 7 pneumonia Epidemic keratoconjunctivitis 8, 19, 37 Pneumonia with dissemination, urinary 5, 31, 34, 35, tract infection 39, 42-47 CNS disease including encephalitis 7, 12, 32 Types 1, 2, 5 and 6 are frequently isolated from the situ tonsils and adenoids of young children. The children may be asymptomatic or may have upper respiratory infection at the time of isolation. Type 3, 4 and 7 are most frequently isolated from young adults with acute upper and lower respiratory disease. Military recruits seem particularly likely to be infected with these agents, as they are to be infected with mycoplasmal and meningococcal organisms. The reasons for the increased infection rates are probably related to the crowding of a susceptible population. Respiratory Tract Infection Faculty Copy – Page 17 STUDY QUESTIONS 1. Describe the modes of adenoviral transmission. Adenoviruses causing respiratory tract infection usually are transmitted by respiratory tract secretions through person-to-person contact, fomites, and aerosols. Because adenoviruses are stable in the environment, fomites may be important in their transmission. The conjunctiva can provide a portal of entry. Community outbreaks of adenovirus-associated pharngonconjunctival fever have been attributed to exposure to water from contaminated swimming pools and fomites, such as shared towels. Epidemic keratoconjunctivitis often has been associated with nosocomial transmission in ophthalmologists’ offices. Enteric strains of adenoviruses are transmitted by the fecal-oral route. Nosocomial spread often has resulted from exposure to contaminated hands of health care workers and infected equipment, including pneumotonometers and opthalmologic solutions. 2. Describe the clinical manifestations of adenoviral infections. The most common site of adenovirus infection is the upper respiratory tract. Manifestations include symptoms of the common cold, pharyngitis, pharyngoconjunctival fever, tonsillitis, otitis media, keratoconjunctivitis, often associated with fever. Life-threatening disseminated infection, severe pneumonia, meningitis, and encephalitis occasionally occur, especially among young infants and immunocompromised hosts. Adenoviruses are infrequent causes of acute hemorrhagic conjunctivitis, a pertussis-like syndrome, croup, bronchiolitis, hemorrhagic cystitis, and genitourinary tract disease. In children, the best described syndrome attributed to adenoviruses is the so-called pharyngoconjunctival fever. This disease occurs in small outbreaks and seen by physicians at children’s summer camps. It is characterized by conjunctivitis, pharyngitis, rhinitis, cervical adenitis, and temperatures to 380C. The onset is acute, and the fever and other symptoms last 3-5 days. Bulbar and palpebral conjunctivitis may be the only finding, and the palpebral conjunctivae usually have a granular appearance. A few adenovirus serotypes, types 40 and 41, have been associated with gastroenteritis, and are responsible for about 4% of serious diarrhea in infants and children. The predominant cause of exudative tonsillitis in infants and toddlers is of adenoviral etiology. Respiratory Tract Infection Faculty Copy – Page 18 3. What is known about the pathogenesis of adenoviral infections? The oropharyngeal and nasopharyngeal mucous membranes are the tissues primarily affected early in acute infection. Adenoviruses appear to be capable of at least three types of interaction with cells. 1) The first is a lytic infection in which the virus goes through an entire replicative cycle. Lytic infection occurs in human epithelial cells and results in cell death and in the production of 10,000 – 1 million progeny viruses per cell, of which 1-5 percent are infectious. 2) The second interaction is a latent or chronic infection. This usually involves lymphoid cells. During latent infection, only small numbers of viruses may be released, and cell death may be outstripped by cell multiplication, thereby resulting in inapparent infection. The mechanisms are not clearly established. 3) The third significant virus – cell interaction occurring with adenoviruses is that of oncogenic transformation. In this situation, only the early steps in virus replication occur. The viral DNA is apparently integrated into and replicated with the cell’s DNA, but no infectious virions are produced. In all three types of infection, virus-specific proteins (T antigens) are synthesized. These antigens give evidence of adenoviral presence even in the absence of infectious virus. The T antigens are detected either by complement fixation or by immunofluorescence assays using serum from hamsters bearing tumors induced by adenovirus. 4. What type of isolation should the patient be in while in the hospital? For young children with respiratory tract infection, contact and droplets precautions are indicated for the duration of hospitalization. For patients with conjunctivitis, contact precautions in addition to standard precautions are recommended. For diapered and incontinent children with adenoviral gatroenteritis, contact precautions in addition to standard precautions are indicated for the duration of the illness. 5. How is the viral infection detected? Detection of adenovirus infection by culture or antigen is the preferred diagnostic method. Respiratory Tract Infection Faculty Copy – Page 19 Adenoviruses associated with respiratory tract disease can be isolated from pharyngeal secretions, eye swabs, and feces by inoculation of specimens into a variety of cell cultures. A pharyngeal isolate is more suggestive of recent infection than is a fecal isolate, which may indicate either prolonged carriage or recent infection. Adenovirus antigens can be detected in body fluids of infected persons by immunoassay techniques, which are especially useful for diagnosis of diarrheal disease, because enteric adenovirus types 40 and 41 usually cannot be isolated in standard cell cultures. Enteric adenoviruses also can be identified by electron microscopy of stool specimens. Multiple methods to detect group-reactive hexon antigens in body secretions and tissue have been developed. Also, detection of viral DNA can be accomplished with genomic probes, synthetic oligonucleotide probes, or gene amplification by polymerase chain reaction. Serodiagnosis is based on detecting a 4-fold or greater rise in antibodies to a common adenovirus antigen (eg, hexon). Serodiagnosis is used primarily for epidemiologic studies. 6. Describe the measures for prevention of the spread of adenoviral infection. Adequate chlorination of swimming pools is recommended to prevent pharyngoconjunctival fever. Epidemic keratoconjunctivitis associated with ophthalmologic practice can be difficult to control and requires use of single-dose medication dispensing and strict attention to hand washing and instrument sterilization procedures. Effective disinfection can be accomplished by immersion of contaminated equiment in a 1% solution of sodium hypochlorite for 10 minutes or by steam autoclaving. Health care personnel with known or suspected adenoviral conjunctivitis should avoid direct patient contact for 14 days after the onset of disease in their second eye. Because adenoviruses are particularly difficult to eliminate from skin, fomites, and environmental surfaces, assiduous adherence to hand washing and use of disposable gloves when caring for infected patients are recommended. Children who participate in group child care, particularly children from 6 months through 2 years of age, are at increased risk of adenoviral respiratory tract infections and gastroenteritis. Measures for preventing spread of adenovirus infection in this setting have not been determined, but frequent hand-washing is recommended. Respiratory Tract Infection Faculty Copy – Page 20 CASE 1 Slide 1 Mild RSV pneumonia There are mild peribronchial infiltrates and the lungs are hyperinflated because of air trapping (air gets in but can’t get out ) because of mucous necrotic debris in the airways. Slide 2 Lateral view of Slide 1 Shows that the lungs are hyperinflated because diaphragms are flattened. Slides 3 - 5 Increasingly progressive RSV pneumonia in infants with congenital heart disease. There are patchy infiltrates and hyperinflation from air trapping. The presence of infiltrates is common in severe RSV pneumonia and does not imply the presence of a secondary bacterial pneumonia. Respiratory Tract Infection Faculty Copy – Page 21 OPTIONAL ARTICLES FOR RESPIRATORY VIRUSES CASE STUDIES II Respiratory Tract Infection Faculty Copy – Page 22 1. RSV Bronchiolitis (1997)-American Family Physician, Vol. 55:1139-1146. 2. Respiratory Syncytial Virus Infection: Indications for the use of Palivizumab and Update on the use of RSV-IG IV. (1998) Pediatrics 102:1211-1216. 3. Croup: An 11 year Study in a Pediatric Practice. (1983) Pediatrics, Vol 71:871-876. 4. A comparison of Nebulized Budesonide, Intramuscular Dexamethasone and Placebo for Moderately Severe Croup. (1998) NEJM 339:498-503. 5. Epstein-Barr Virus Infection (2000). NEJM 343:481-492. 6. Inhaled Zanamivir for the Prevention of Influenza in Families (2000), NEJM 343:1282-1289. 7. Drug Therapy: Prevention and treatment of Influenza (2000). NEJM 343:1778-1787. *****