05/20/2008 Kathy`s Indwelling Catheter Indications and Care Fact
advertisement
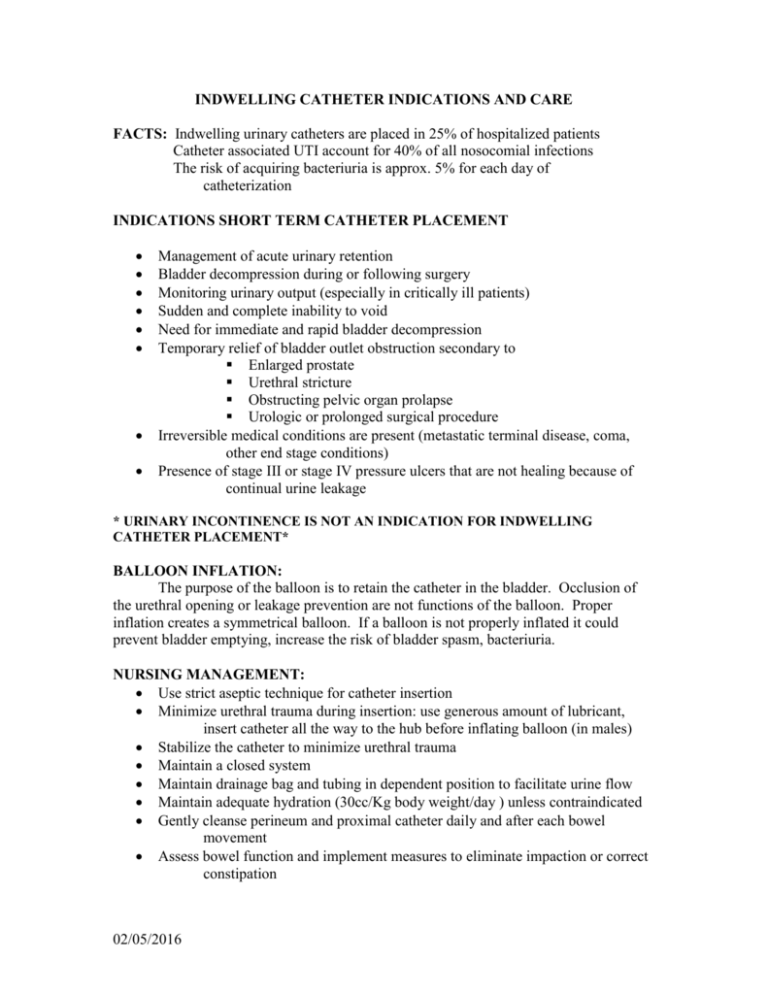
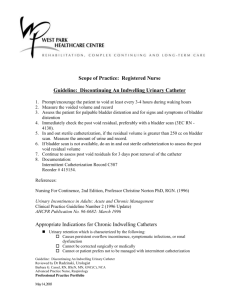
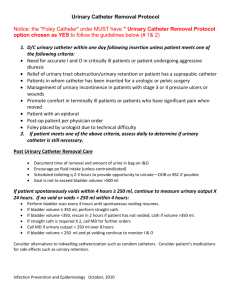
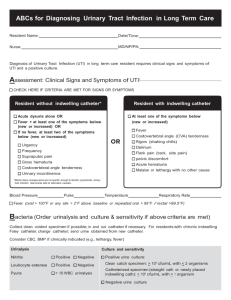
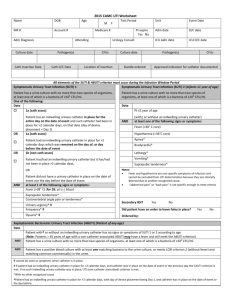
INDWELLING CATHETER INDICATIONS AND CARE FACTS: Indwelling urinary catheters are placed in 25% of hospitalized patients Catheter associated UTI account for 40% of all nosocomial infections The risk of acquiring bacteriuria is approx. 5% for each day of catheterization INDICATIONS SHORT TERM CATHETER PLACEMENT Management of acute urinary retention Bladder decompression during or following surgery Monitoring urinary output (especially in critically ill patients) Sudden and complete inability to void Need for immediate and rapid bladder decompression Temporary relief of bladder outlet obstruction secondary to Enlarged prostate Urethral stricture Obstructing pelvic organ prolapse Urologic or prolonged surgical procedure Irreversible medical conditions are present (metastatic terminal disease, coma, other end stage conditions) Presence of stage III or stage IV pressure ulcers that are not healing because of continual urine leakage * URINARY INCONTINENCE IS NOT AN INDICATION FOR INDWELLING CATHETER PLACEMENT* BALLOON INFLATION: The purpose of the balloon is to retain the catheter in the bladder. Occlusion of the urethral opening or leakage prevention are not functions of the balloon. Proper inflation creates a symmetrical balloon. If a balloon is not properly inflated it could prevent bladder emptying, increase the risk of bladder spasm, bacteriuria. NURSING MANAGEMENT: Use strict aseptic technique for catheter insertion Minimize urethral trauma during insertion: use generous amount of lubricant, insert catheter all the way to the hub before inflating balloon (in males) Stabilize the catheter to minimize urethral trauma Maintain a closed system Maintain drainage bag and tubing in dependent position to facilitate urine flow Maintain adequate hydration (30cc/Kg body weight/day ) unless contraindicated Gently cleanse perineum and proximal catheter daily and after each bowel movement Assess bowel function and implement measures to eliminate impaction or correct constipation 02/05/2016 MANAGE/PREVENT LEAKAGE Assess for patency, if occluded remove and replace Assess for signs and symptoms of UTI ( to obtain urine for culture, remove existing catheter and replace before obtaining sample) If urine is concentrated, provide adequate hydration (unless contraindicated) Check for fecal impaction, remove if present, institute bowel management program Check for proper balloon inflation Stabilize catheter For severe bladder spasms, consider MD consult for anticholinergics CDC RECOMMENDATIONS “Urinary catheterization should be discouraged as a means of obtaining urine for culture or certain diagnostic tests such as urinary electrolytes when the patient can voluntarily void or as a substitute for nursing care of the incontinent patient”. 02/05/2016 REFERENCES Cochran, S. Care of the indwelling urinary catheter: Is it evidence based? Journal of Wound, Ostomy and Continence Nursing. 2007;34(3):282-288. Gray, M. What nursing interventions reduce the risk of symptomatic urinary tract infection in the patient with an indwelling catheter? Evidence-Based Report Card from the Center for Clinical Investigation. Journal of Wound, Ostomy and Continence Nursing. 2004;31(1):3-13. Newman, DK. The indwelling urinary catheter: Principles for best practice. Journal of Wound, Ostomy and Continence nursing. 2007;34(6):655-661. Wong, E.S., Hooten, T.M. Guideline for prevention of catheter-associated urinary tract infection. http://www.cdc.gov/ncidod/dhqp/gl_catheter_assoc.html. Wound, Ostomy and Continence Nurses Society. Clinical fact sheet: Indwelling catheters:http://www.wocn.org. 02/05/2016