Respiratory
advertisement
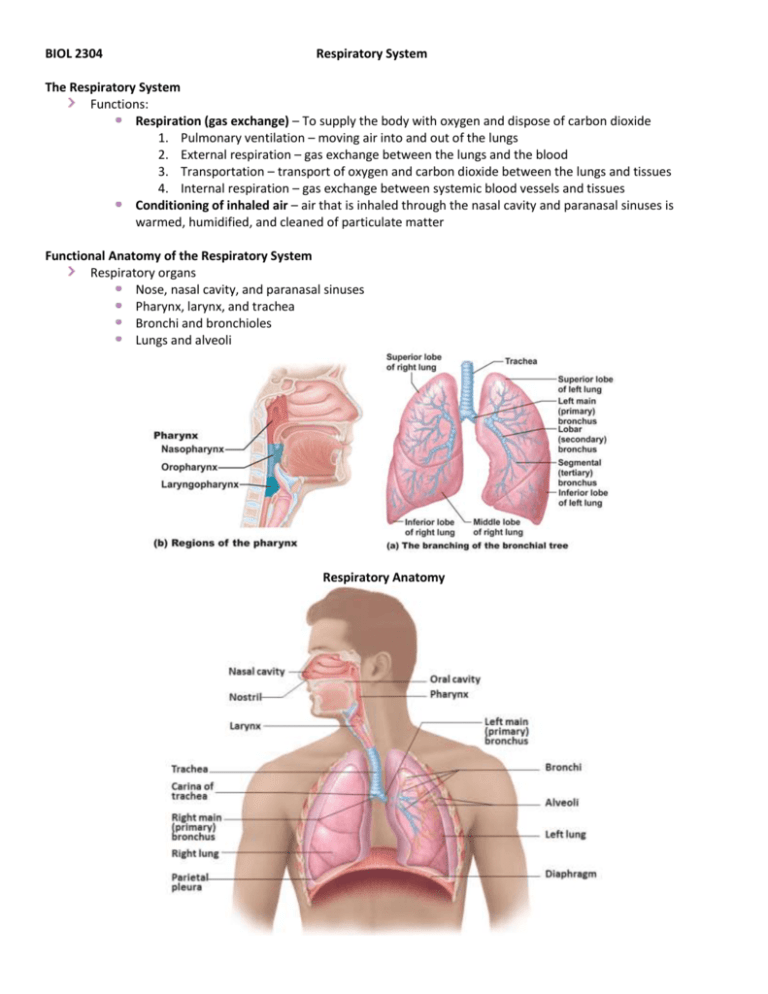
BIOL 2304 Respiratory System The Respiratory System Functions: Respiration (gas exchange) – To supply the body with oxygen and dispose of carbon dioxide 1. Pulmonary ventilation – moving air into and out of the lungs 2. External respiration – gas exchange between the lungs and the blood 3. Transportation – transport of oxygen and carbon dioxide between the lungs and tissues 4. Internal respiration – gas exchange between systemic blood vessels and tissues Conditioning of inhaled air – air that is inhaled through the nasal cavity and paranasal sinuses is warmed, humidified, and cleaned of particulate matter Functional Anatomy of the Respiratory System Respiratory organs Nose, nasal cavity, and paranasal sinuses Pharynx, larynx, and trachea Bronchi and bronchioles Lungs and alveoli Respiratory Anatomy Respiratory System Consists of: Respiratory muscles – Diaphragm contracts for inspiration, relaxes for expiration External intercostal muscles contract for inspiration Internal intercostal muscles contract for forced expiration Smooth muscle surrounding bronchioles and pulmonary capillaries Conducting zones Nose, nasal cavity, pharynx, trachea, bronchi, terminal bronchioles Provides rigid conduits for air to reach the sites of gas exchange Air passages undergo 23 orders of branching in the lungs Respiratory zone – site of external respiration Respiratory bronchioles, alveolar ducts, alveolar sacs, alveoli The Nose Provides an airway for respiration Moistens and warms air Filters inhaled air Resonating chamber for speech Houses olfactory receptors Skin is thin – contains many sebaceous glands The Nasal Cavity External nares – nostrils Divided by nasal septum Vestibule - anterior opening of nares Continuous with nasopharynx Two mucous membranes: Olfactory mucosa - near roof of nasal cavity, houses olfactory (smell) receptors Respiratory mucosa - lines nasal cavity Pseudostratified ciliated columnar epithelium Goblet cells within epithelium Cilia move contaminated mucus posteriorly to be swallowed Nasal Cavity Nasal Conchae 3 paired bony projections along the lateral walls of the nasal cavity Superior and middle nasal conchae – part of the ethmoid bone Inferior nasal conchae –individual bone Function: Deflect particulate matter onto mucus-coated surfaces The Paranasal Sinuses The Pharynx Funnel-shaped passageway Extends from base of skull to esophagus Connects nasal cavity with oral cavity Type of mucosal lining changes along its length Divided into three sections: Nasopharynx – between base of skull and soft palate Oropharynx – posterior to oral cavity Laryngopharynx – between the hyoid bone and the esophagus The Nasopharynx Superior portion of pharynx Air passageway only (closed off during swallowing) Epithelium consists of pseudostratified ciliated columnar epithelium that moves mucus Pharyngeal tonsil (adenoids) Located on posterior wall, destroys entering pathogens Contains the opening to the auditory tube Tubal tonsil - located posterior to the opening of the Eustachian tube; provides some protection from infection The Nasopharynx The Oropharynx Fauces - the arch-like entranceway from the oral cavity into the oropharynx Oropharynx extends from soft palate to the epiglottis Epithelium: stratified squamous epithelium Two types of tonsils in the oropharynx Palatine tonsils – in the lateral walls of the fauces Lingual tonsils – covers the posterior surface of the tongue The Laryngopharynx Passageway for both food and air Epithelium: stratified squamous epithelium Continuous with the esophagus and larynx The Larynx Passageway for air only Prevents food and drink from entering the trachea Produces vocal sounds Connects the pharynx to the trachea Epithelium of the larynx Superior portion: Stratified squamous Inferior portion: Pseudostratified ciliated columnar Nine Cartilages of the Larynx Three unpaired cartilages: Thyroid cartilage - shield-shaped, forms laryngeal prominence (Adam’s apple) Epiglottis - tips inferiorly during swallowing Cricoid cartilage - a ring of hyaline cartilage that forms the inferior wall of the larynx Three smaller, paired cartilages: Arytenoid cartilages Corniculate cartilages Cuneiform cartilages The Larynx Vocal ligaments of the larynx Vocal folds (true vocal cords) - act in sound production Vestibular folds (false vocal cords) - no role in sound production Voice production Length of the vocal folds changes with pitch Loudness depends on the force of air across the vocal folds The Larynx The Trachea Descends into the mediastinum C-shaped cartilage rings keep airway open Carina - marks where trachea divides into two primary bronchi Epithelium: pseudostratified ciliated columnar Bronchi in the Conducting Zone Bronchial tree - extensively branching respiratory passageways Primary bronchi (main bronchi) Largest bronchi Right main bronchi - wider and shorter than the left Secondary (lobar) bronchi Three on the right Two on the left Tertiary (segmental) bronchi - branch into each lung segment Bronchioles - little bronchi, less than 1 mm in diameter Terminal bronchioles - less than 0.5 mm in diameter Tissue Composition of Conducting Zone Changes along pathway Supportive connective tissues change C-shaped rings – trachea, primary bronchi Replaced by cartilage plates (secondary, tertiary, and smaller bronchi) Epithelium changes Trachea pseudostratified ciliated columnar Bronchi: simple columnar epithelium Bronchioles and terminal bronchioles: simple cuboidal epithelium Smooth muscle in bronchioles becomes important Airways widen with sympathetic stimulation Airways constrict under parasympathetic direction Lobes, Fissures, & Markings of the lungs Left lung: Two lobes – Superior and inferior lobes Fissure – oblique Right lung: Three lobes: Superior, middle, and inferior Fissures – oblique and horizontal Major landmarks: Apex, base, hilum, and root Bronchi and vasculature enter the lungs at the hilum Cardiac notch – concavity on medial surface The Pleurae A double-layered sac surrounding each lung Parietal pleura – lines pleural cavity wall Visceral pleura – covers lungs Pleural cavity - potential space between the visceral and parietal pleurae Pleurae help divide the thoracic cavity Central mediastinum Two lateral pleural compartments Structures of the Respiratory Zone Consists of air-exchanging structures Respiratory bronchioles – branch from terminal bronchioles Lead to alveolar ducts Lead to alveolar sacs Alveolar Sacs Features Of Alveoli Structure of Alveoli Respiratory membrane - alveolar and capillary walls plus their basal lamina Type I cells Single layer of simple squamous epithelial cells Surrounded by basal lamina Type II cells – scattered among type I cells Are cuboidal epithelial cells Secrete surfactant – reduces surface tension within alveoli Alveolar macrophages Features Of Alveoli Surrounded by elastic fibers Interconnect by way of alveolar pores Internal surfaces A site for free movement of alveolar macrophages Transverse section Pulmonary Ventilation During inspiration/inhalation Diaphragm contracts and flattens Intercostal muscle contract and raise ribs Volume of thoracic cavity increases During expiration/exhalation Inspiratory muscles relax Volume of thoracic cavity decreases Muscles of Pulmonary Ventilation Neural Anatomy of Breathing System Most important respiratory center Ventral Respiratory Group (VRG) Located in reticular formation in the medulla oblongata Neurons generate respiratory rhythm