Back Pain in a Gymnast
advertisement

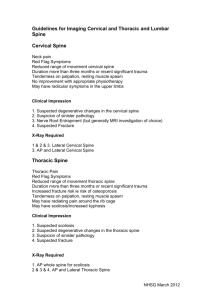
Back Pain in a Gymnast An understanding of its cause and treatment David Kruse, M.D. Former Senior Men’s National Team Member USAG Men’s National Team Physician Assistant Clinical Professor & Director of Primary Care Sports Medicine University of California, Irvine Sibylle Mehta, P.T. Former Austrian Women’s Senior National Team Member & 3 time Austrian National Champion Physical Therapist (DPT Candidate), Orange County, CA Introduction As we all know, gymnastics requires a level of fitness and total body control that is rarely matched by other sports. As a result, there are many different injuries that can hamper a gymnast’s training, competition schedule, and ultimately their career. In particular, the back can be a common source of injury in gymnastics. Back pain has long been recognized as a major reason for doctor visits. This results in medical costs amounting to billions of dollars annually.1,2 Recently, more attention has been brought to the high prevalence of back pain in children, more common than previously thought, with multiple medical studies showing back pain in 30-50% of adolescents studied.3,4,5 In many sports, including gymnastics, the prevalence of low back injury is even higher.6,7,8,9 Studies have shown that in female and male artistic gymnasts the rates of low back pain can be as high as 75% to 85%, respectively.10 For rhythmic gymnasts, one study published in 1999 showed reports of low back pain in 86% of the gymnasts studied.11 Consequently, for coaches and parents, it is important to know how to recognize back pain, common causes, and how to facilitate the full recovery of your gymnasts. Understanding Back Pain Before you begin to understand your gymnast’s back pain, you need to have a grasp of the anatomy of the back and how it works. The low back, or lumbar spine, is composed of 5 vertebrae, L1 through L5, and are stacked in between the thoracic vertebrae above and the sacrum below. In between each vertebra lies an intervertebral disc, a fluid-filled sac. The spinal column lies behind the vertebral body and discs, through which the nerves from the spinal cord run. The nerves leave the spinal column between each vertebra and control the sensation and strength of our lower body, including pain. (Figure 1) Surrounding the spinal structures are muscles, running up and down and in the front and back of the spine, that provide support and stability. In brief, these include the abdominal and psoas muscles in front and the erector spinae muscles in back. The spine allows for the trunk to flex (forward bend), extend (back bend), side flex (side bend), and rotate (twist). Most of these occur at the joints of the back, called facet joints. The flexion and extension of the spine occurs mostly at the lower two lumbar vertebrae, L4 and L5. Combined movements, such as extension with rotation, as well as repetitive movements have the highest potential for injury.12 With this knowledge; it starts to become obvious why many gymnasts suffer from low back pain. How to Recognize Low Back Pain Depending on the cause of the back pain, your gymnast may complain of a variety of different symptoms. Most commonly for gymnasts, though, onset is gradual and with activity, worse with extension (back bend) of the lumbar spine. The pain can be on one or both sides of the low back and will sometimes be associated with buttock pain. This article will focus on the common causes of back pain in gymnasts but it is important to know how to recognize signs of more dangerous causes of back pain for which your athlete should seek more immediate medical attention. These would include: fever, loss of balance, numbness or weakness, and loss of control of urine or stool. In addition, constant pain not related to their gymnastics activity and night pain should prompt a more immediate doctor’s visit.6,13,14 Causes of Low Back Pain There are many possible causes of back pain in children. A condition called spondylolysis, in particular, has been recognized as a very common source of low back pain in the adolescent sports population and is a common cause of these symptoms in gymnasts.9,15,16 The following discussion will focus on spondylolysis, as well as an associated injury, spondylolisthesis. Other possible causes of low back pain in gymnasts will be briefly mentioned. Spondylolysis and Spondylolisthesis We should start by discussing the definition of these conditions to better understand how injury happens and pain and disability begins. Spondylolysis can be defined as a defect or stress fracture of a part of the vertebra (back bone) near where one vertebra connects to another. This can occur on one or both sides of a vertebra. Spondylolisthesis is a slippage of one vertebra on another.6 (Figure 2) The commonality of spondylolysis in children is becoming more recognized and one medical study showed that 5% of children by the age of 6 will have this back defect.17 The Team Physician’s Handbook, states an even higher incidence for female gymnasts, citing a probable 10-11% incidence, and possibly an even higher risk in rhythmic gymnastics.6 This type of injury usually is a result of repeated hyperextension, hence the increased incidence in gymnastics. As mentioned, the greatest degree of extension occurs at L4 and L5 and consequently the majority of spondylolysis injuries will occur in this area of the spine. Your gymnast will complain of back pain at the site of injury or fracture and will sometimes be associated with buttock pain. The symptoms are activity-related. Common skills that might exacerbate spondylolysis injuries are: back walkover or back handspring, vaulting skills (especially yurchenko), any rebounding or punching skill, ring giant swing, release-move tap, and dismount landings, to name a few. If these symptoms are identified in your gymnast, the next step should be an evaluation by their physician. Their doctor will ask detailed questions regarding the history of the injury and complete a comprehensive exam. Initial evaluation will usually include simple back x-rays. The clinician may then choose more advanced studies including SPECT (single photon emission computed tomography) scan, thin-cut CT scan or MRI of the lumbar spine.6,9 Depending on the results of the imaging studies and if a diagnosis of spondylolysis is given, your gymnast will need a structured treatment plan, as discussed below. If a spondylolysis injury occurs on both sides of the vertebral bone, this may lead over time to the slippage of one vertebra on another, resulting in spondylolisthesis. Simple x-rays can identify this. Other Causes of Back Pain The following is a brief discussion of other causes of back pain in gymnasts. The goal should be to familiarize yourself with these so you are aware of other conditions your athlete may suffer from: Nonspecific back pain (Mechanical Back Pain)– An exact diagnosis for back pain may not be found in up to 78% of children and consequently your athlete’s doctor may not be able to provide an exact reason for the back pain. 13,18 A thorough examination is important to find out what muscles may be too weak and/or too tight, which may be the cause of this pain. Facet Syndrome – The facet joints are where one vertebrae moves on another. Just like any other joint in the body, the facet joints can become aggravated causing pain. This, like spondylolysis, usually occurs from forceful extension and rotation motions.14 Scoliosis – This is an abnormal side-to-side curvature of the spine that is routinely screened for during doctor well-child visits, as well as in schools. Among children who have scoliosis, 30% will have back pain. Children who have pain from scoliosis typically have a history of trauma or a fall.19 Meaning, a couple falls from the beam or high bar may unmask previously undiagnosed scoliosis. Other potential causes: Intervertebral disc injury, herniated vertebral disc, vertebral growth plate injury, and Scheuermann’s disease.9,13,20 Life-threatening causes: Diskitis, Osteomyelitis, and Cancer. These are rare but can result in more serious outcomes.13,20 Treatment As a coach or parent, it is important to have a good understanding of the initial treatment and subsequent rehabilitation that is necessary for a back injury. This will ensure that your expectations for when your athlete returns to full activity are accurate and safe for the athlete. The treatment discussed here will be focused on the management of spondylolysis. All of the principles listed below should be planned and implemented by your athlete’s medical team, i.e. physician, physical therapist, certified athletic trainer, chiropractor, etc. Initial Treatment Pain from a spondylolysis injury will usually resolve if the athlete’s activity is modified. However, if no treatment is pursued, it can cause persistent pain and progress to a slipped vertebra. The initial treatment should protect the injured vertebra. This is done by restricting the gymnast’s activity to avoid further irritation of the injury. The athlete’s medical team should dictate activity modification. Together with this modified activity, pain and inflammation can be treated with nonsteroidal anti-inflammatory drugs (as directed by the physician), icing, electro-stimulation, heat therapy after the initial inflammation has resolved, and acupuncture. The doctor may elect to put your gymnast in a special brace to help control pain and promote healing. Initial therapeutic exercises are focused on controlling pain, avoiding loss of strength, and restoring overall function. These exercises should be done under the direction of a licensed physical therapist or certified athletic trainer.9,14,21 Rehabilitation As pain lessens, your athlete will be progressed through a more intensive therapy program. In general, the rehabilitation program is divided into three different stages.22 The first stage, as mentioned above, focuses on controlling pain and inflammation through modification of activity. Taking pressure off the spine will help the recovery process. Have your gymnast lie on their back with the hips and knees bent at 90 degrees. Ice and heat can be used as needed. Your gymnast can also perform isometric abdominal squeezes (during which the muscles contract against resistance but movement of the spine is avoided), even if wearing a brace, as long as there is no pain. The second stage focuses on regaining pain-free range of motion, improving strength and function of the lumbar spine, and improving strength and flexibility of the legs. There is also a focus on correcting deficits in posture, flexibility, and mechanics that would predispose your gymnast to develop a recurrence of the injury or pain. It is important to understand that your gymnast is expected to regain excessive range of motion after the injury and must be conditioned to regain the strength and endurance necessary to control this motion. 23 Adjacent joints must also be assessed for lack of flexibility and strength. The spine may be overstressed as a result of insufficient motion or strength of the surrounding joints. For example, insufficient ankle range of motion and quadriceps strength can cause the impact from landing to travel up to the spine and increase your gymnast’s symptoms.24 Components of the strength program are: (a) increase the muscular stability of the spine 24,25, (b) increase the ability of the low back to handle muscular conditioning, (c) restore muscle size, strength, and endurance, (d) reestablish coordinated muscle activity, and (e) reduce pain through spine strengthening.24 There are many spine strengthening programs available that a physical therapist can use too heal your gymnast. 23, 24, 25, 26 The last stage of rehabilitation focuses on functional and gymnastics-specific activities. When returning to gymnastics, the rehabilitation program will progress through various levels of dynamic activity. 23 These exercises should be done under the direction of a certified physical therapist or certified trainer. 9,14 An additional component of therapy is to offer rehabilitation while your athlete continues to participate in gymnastics. Often, the gym becomes a second home rather than just a place to train. Participation in the gym allows your athlete to maintain camaraderie with teammates, and participate fully in the visual and verbal training of the sport. Watching other athletes complete skills, and receive feedback, allows them to learn from observation and through that improve their performance quality even when they cannot physically participate. 23 Return to the Mat With athletic injury it is always important to start with a realistic time course of recovery in order to avoid premature return to activity and re-injury. With spondylolysis injury, there is a wide range of possible outcomes. With early recognition and proper rehabilitation, most gymnasts will have excellent outcomes and can return to full activity. The length of time for full recovery is dependent on the initial extent of injury and may vary between 2 and 9 months.9 After full recovery, your gymnast’s doctor may choose to obtain more images of the spine to assess for evidence of bone healing.6,9 Some gymnasts may have a difficult recovery. In these cases of incomplete recovery, there are other options. Bracing has been used in the treatment of these injuries and is considered an effective option in certain cases. Injections and surgical correction is used in extreme cases of persistent symptoms, significant vertebral slipping, or in cases with ongoing weakness and numbness.6,8,9 In routine cases, progression to full activity begins slowly over 4-6 weeks after rehabilitation is complete. When your gymnast returns to gymnastics-specific activities, he/she should be guided by symptoms, i.e. pain. Activity should be reduced or eliminated if pain recurs. Complete lumbar spine function with a lack of symptoms following return to gymnastics-specific activity usually indicates your athlete has had a successful return. It is important to realize, though, that one of the best predictors of low back injury during athletic activity is a previous low back injury. Therefore, a long-term maintenance rehabilitation program should be continued past the resolution of symptoms in order to help prevent a recurrence.6,9,13,14,21 Conclusion As we all know, injury is an inevitable part of gymnastics and dealing with this unfortunate event can be half the battle of preparing your athlete for competition. Therefore, a good understanding of some of the more common injuries seen in gymnastics will provide you with more knowledge and insight to help prevent injury and facilitate recovery if injury does occur. The best chance for your athlete’s eventual full recovery, with the least amount of time lost from training and competition, comes with early diagnosis and treatment. This is true for low back injuries, as well, and I hope that this article has succeeded in making a very common problem more approachable. Good luck in the gym and stay safe. Figure 1: Picture of a vertebra with the appropriate anatomy Figure 2: Picture of a gymnast in extreme lumbar extension Figure 3: Take Home Points 1. Low back pain can occur in approximately 80% of gymnasts. 2. Spondylolysis, a vertebral stress fracture, is a common back injury in gymnastics and occurs with repetitive hyperextension and rotation. 3. Rehabilitation begins with pain control and range of motion, and then progresses to strengthening & functional training. 4. Early diagnosis and treatment with a well-planned rehabilitation program and smart return to full activity, provides your gymnast with the greatest chance for full and efficient recovery. References: 1. Deyo RA, Mirza SK, Martin BI. Back Pain Prevalence and Visit Rates. Spine. 2006;31(23):27242727. 2. Frymoyer JW, Cats-Baril WL. An overview of the incidences and costs of low back pain. Orthop Clin North Am. 1991;22(2):263-271. 3. Olsen TL, et al. The Epidemiology of Low Back Pain in an Adolescent Population. Am J Public Health. 1992;82(4):606-608. 4. Skaggs DL, et al. Back pain and backpacks in school children. J Pediatr Orthop. 2006;26(3):358363. 5. Burton AK. The natural history of low back pain in adolescents. Spine. 1996;21(20):2323-2328. 6. Wilhite JM. Thoracic and Lumbosacral Spine. Team Physician’s Handbook. 3rd ed. Hanley & Belfus, Inc., Philadelphia, 2002:460-479. 7. Sward L, et al. Back pain and radiologic changes in the thoraco-lumbar spine of athletes. Spine. 1990;15:124-129. 8. Micheli LJ. Back Injuries in Gymnastics. Clin Sport Med. 1985;4(1):85-92. 9. Standaert CJ. New strategies in the management of low back injuries in gymnasts. Curr Sports Med Rep. 2002;1(5):293-300. 10. Sward L, et al. Disc degeneration and associated abnormalities of the spine in elite gymnasts. A magnetic resonance imaging study. Spine. 1991;16:437-43. 11. Hutchinson MR. Low back pain in elite rhythmic gymnasts. Medicine & Science in Sports & Exercise. 1999;31(11):1686. 12. Hainline B. Low back injury. Clin Sports Med. 1995;14(1):241-265. 13. Shilt JS, Barnett TM. Evaluating and managing back pain in children. J of Musculoskeletal Medicine. 2007;24(2):73-86. 14. Drezner JA, Herring SA. Managing Low-Back Pain. The Physician and Sportsmedicine. 2001;29(8):37-43. 15. Micheli LJ, Wood R. Back pain in young athletes: significant differences from adults in causes and patterns. Arch Pediatr Adolesc Med. 1995;149:15-18. 16. Goldstein JD, et al. Spine Injuries in gymnasts and swimmers. An epidemiologic investigation. Amer J Sports Med. 1991;19(5):463-468. 17. Cavalier R, et al. Spondylolysis and spondylolisthesis in children and adolescents, I: diagnosis, natural history, and nonsurgical management. J Am Acad Orthop Surg. 2006;14:417-424. 18. Bhatia NN, et al. Diagnostic modalities for the evaluation of pediatric back pain: a prospective study. J Pediatr Orthop. 2008;28(2):230-3. 19. Ramirez N, et al. The prevalence of back pain in children who have idiopathic scoliosis. J Bone Joint Surg. 1997;79A:364-368. 20. Feldman DS, et al. Evaluation of an Algorithmic Approach to Pediatric Back Pain. J Pediatr Orthop. 2006;26(3):353-357. 21. Bono CM. Current Concepts Review: Low-Back Pain in Athletes. J of Bone and Joint Surg. 2004;86A(2):382-396. 22. Nguyen, D.T., Orgill D.P., Murphy G.F. (2009). Chapter 4: The Pathophysiologic Basis for Wound Healing and Cutaneous Regeneration. Biomaterials for Treating Skin Loss. Woodhead Puplishing (UK/Europe) & CRC Press (US), Cambridge/Boca Raton, p. 25-57 23. Hunter-Giordano AO, Pongetti Angeletti GM, Voelker S, Manal TJ. Physical Therapy for the Performing Artist. 2010, Orthopaedic Section, APTA, Inc. 24. Kolber MJ, Beekhuizen K. Lumbar Stabilization: An Evidence-Based Approach for the Athlete with Low Back Pain. Strength and Conditioning Journal. Lawrence: 2007. Vol. 29, Iss. 2 25. O’Sullivan, B.D. Phyty, L.T. Twomey, and G.T. Allison. Evaluation of specific stabilizing exercises in the treatment of chronic low back pain with radiologic diagnosis of spondylosis or spondylolisthesis. Spine. 22: 2959-2967. 1997. 26. McGill SM. Low back exercises: evidence for improving exercise regimens. Phys Ther. 1998; 78(7): 754-765.