METABOLIC DISEASE
advertisement
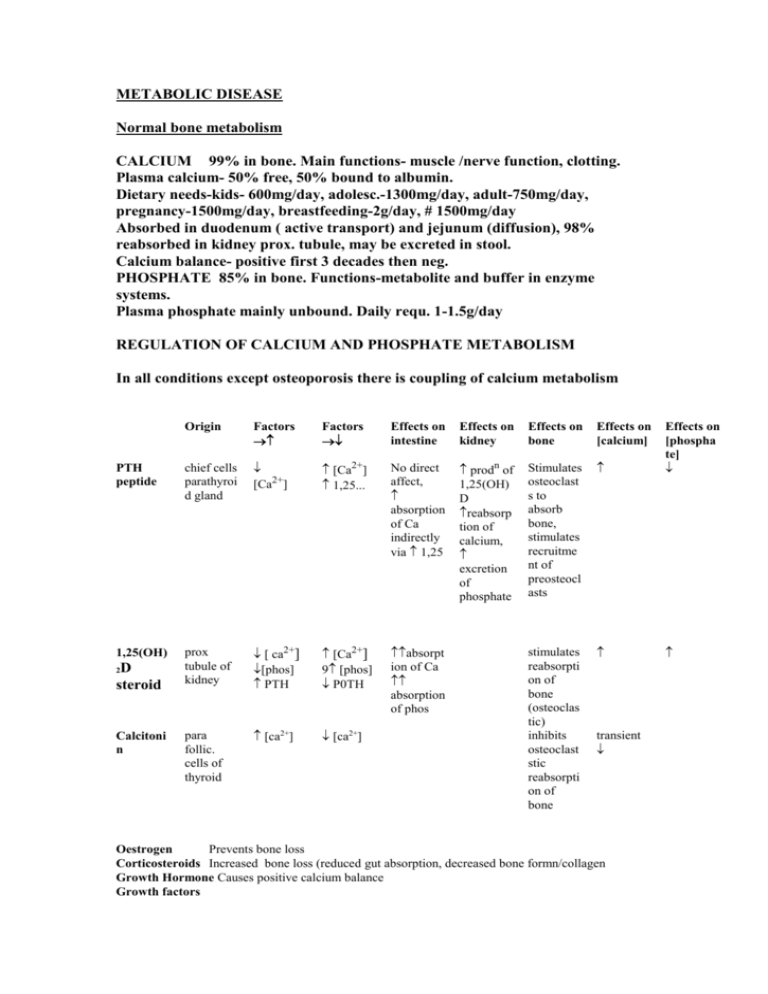
METABOLIC DISEASE Normal bone metabolism CALCIUM 99% in bone. Main functions- muscle /nerve function, clotting. Plasma calcium- 50% free, 50% bound to albumin. Dietary needs-kids- 600mg/day, adolesc.-1300mg/day, adult-750mg/day, pregnancy-1500mg/day, breastfeeding-2g/day, # 1500mg/day Absorbed in duodenum ( active transport) and jejunum (diffusion), 98% reabsorbed in kidney prox. tubule, may be excreted in stool. Calcium balance- positive first 3 decades then neg. PHOSPHATE 85% in bone. Functions-metabolite and buffer in enzyme systems. Plasma phosphate mainly unbound. Daily requ. 1-1.5g/day REGULATION OF CALCIUM AND PHOSPHATE METABOLISM In all conditions except osteoporosis there is coupling of calcium metabolism Origin Factors Factors Effects on intestine Effects on kidney Effects on bone Effects on [calcium] PTH peptide chief cells parathyroi d gland [Ca2+] [Ca2+] 1,25... No direct affect, absorption of Ca indirectly via 1,25 prodn of 1,25(OH) D reabsorp tion of calcium, excretion of phosphate Stimulates osteoclast s to absorb bone, stimulates recruitme nt of preosteocl asts Effects on [phospha te] 1,25(OH) prox tubule of kidney [ ca2+] [phos] PTH [Ca2+] 9 [phos] P0TH absorpt ion of Ca absorption of phos para follic. cells of thyroid [ca2+] [ca2+] stimulates reabsorpti on of bone (osteoclas tic) inhibits osteoclast stic reabsorpti on of bone D steroid 2 Calcitoni n transient Oestrogen Prevents bone loss Corticosteroids Increased bone loss (reduced gut absorption, decreased bone formn/collagen Growth Hormone Causes positive calcium balance Growth factors Insulin like growth factor; produced by osteoblasts, recruits osteoblasts Transforming Growth factors; produced during bone resorption, stimulate osteoblasts IL1 and osteoclast activating factor; activate bone resorption Prostaglandins; regulate both osteoblasts and osteoclasts Metabolism of Vit D Diet 7 Dehydrocholesterol skin Vit D3 (Cholecalciferol) liver 25-OH-Cholecalciferol kidney 1,25 dihydroxycholecalciferol 24,25 dihydroxycholecalciferol (inactive) Bone (absorption of bone) Small intestine (absorption of calcium) Disorders of Bone Mineralisation Hypercalcaemia Symptoms- ‘bones, moans, stones and abdominal groans’polyuria, constipation,lethargy,disorientation,bony resorption+/- figrous replacement(osteitis fibrosa cystica),weakness,CNS effects. Primary hyperparathyroidismAge40-65 F:M2:1 Pathology Adenoma/hyperplasia Clinical features often asymptomatic, only 10% have bone disease Moans, bones stones and abdominal groans Xrays osteopenia, osteitisfibrosa cystica,brown tumours, subperiosteal erosions (phalanges),pathological fractures. Calcification of soft tissues Blood results calcium, PTH, phosphate, alk. phosp. N/( increased with osteitis fibrosa Treatment Parathyroidectomy beware hungry bone syndrome post op, (hypocalcaemia due to brisk formn of new bone) Secondary hyperparathyroidism Parathyoid over secretion is a predictable response to chronic hypocalcaemia. Therefore found in rickets and osteomalacia, accounting for some of radiological findings Other causes of Hypercalcaemia MENMalignancy,hyperthyroidism, addisons, steroids, peptic ulcers, kidney disease, sarcoidosis Hypocalcaemia Causes neuromuscular instability (tetany, seizures, Chvostek’s sign). Cataracts,fungal nail infections, Prolonged QT on ECG Caused by low PTH or low Vit D Primary hypoparathyroidism Causes; can be iatrogenic after thyroidectomy Clinical Features; fungal infections of nails, hair loss, vitiligo Xrays; skull Xrays, calcification of basal ganglia Blood results; low calcium, high phosphate Pseudo hypoparathyroidism eg. Albright hereditary osteodystrophy Incidence; rare Pathology; genetic x linked dominant.lack of effect of PTH at target cell. Clinical features; obesity, diminished intelligence, short 1st 4th, 5th metacarpals and metatarsals, exostoses, brachydactyly. Blood tests; normal or high PTH, low Ca, high phosphate Renal Osteodystrophy Pathology; chronic renal failure, leads to failure to excrete phosphate, ass. with long term dialysis. Chronic renal disease Glomerular damage uremia Tubular damage phosphate retention Hyperphosphatemia Ectopic calcification reduced synthesis of 1,25(OH)D3 reduced GI absorption of calcium Increased serum calcium secondary hyperparathyroidism Hypocalcaemia rickets/osteomalacia osteitis fibrosa osteosclerosis xrays; Blood tests; Treatment; rugger jersey spine, soft tissue calcification calcium normal or low, abnormal renal function, raised alk phos., aimed at kidney disease Rickets/ osteomalacia in adults Failure of mineralisation of bone Causes; Nutritional deficiency- vit D chelators of calcium- phytates, chelates phosphorous Antacid abuse, causing reduced dietary phosphate binding GI Absorption defects- Post gastrectomy Biliary disease (reduced absorption of ADEK) Small bowel disease liver disease Renal tubular defects Renal osteodystrophy Miscellaneous causes Clinical features; Rickets tetany , convulsions, failure to thrive, listlessness, muscular flaccidity. Flattening of skull(craniotabes), thickening of wrists from epiphyseal overgrowth, bow legs, stunted growth, rickety rosary, spinal curvature, coxa vara, bowing, # of long bones Osteomalacia, aches and pains, muscle weaknessloss of height, stress #s Xray findings: Rickets; Thickening and widening of physes, cupping of metaphysis, bowing of diaphysis, wide metaphysis. Osteomalacia; Loosers zones- incomplete stress # with healing lacking calcium, on compression side of long bones. Codfish vertebrae due to pressure of discs, trefoil pelvis, due to indentation of acetabulae, stress #s + the Xray changes of 2ndary hyperparathyroidism Blood tests; Reduced calcium, reduced phosphate, increased alk. Phos. Diminished urinary excretion of calcium,In vit D deficient rickets, 25 hcc also low. Calcium phosphate productis normally 3. In rickets and osteomalacia is less than 2.4 eg.Vit D deficient rickets; Due to lack of vit D Histology- Swiss cheese trabeculae and widened osteoid seams gross distortion at maturation zone of physis, poorly defined zone of calcification Treatment- vitamin D (5000u) and Calcium (3g/day) e.g. Hereditary vit D dependent rickets; Rare Autosomal recessive Defect in 1 hydroxylation of vit D3 in kidney causing reduced 1,25 dihydroxy cholecalciferol Clinical features; similar to other causes of rickets but can be worse + baldness Treatment; High levels of vit D e.g. Vitamin D resistant rickets/ familial hypophosphataemic rickets; X linked dominant Impaired renal tubular reabsorption of phosphate clinical features; similar to other types Treatment; phosphate and vit D replacement e.g Hypophosphatasia AR Disorder Low levels of alk phos. (makes inorg phospate, important for bone matrix formn) Diagnosis, increased urinary phosphoethanolamine Treatment, Phosphate therapy Ideopathic Juvenile osteoporosis Incidence; Age Pathology; Blood tests; Prognosis; rare 8-14 Osteopenia, growth arrest normal calcium and phosphate spontaneous resolution Osteopetrosis Mild form AD, malignant form AR Pathology; Failure of osteoclastic and chondroclastic resorption secondary to defect in thymus producing dense bone Xrays; Rugger Jersey spine, marble bone, ‘Erlenmyer flask’prox humerus, /distal femur Treatment; Bone marrow transplant for malignant cases Infantile Cortical Hyperostosis (Caffey syndrome) Age; 0-9 months Pathology; Soft tissue swelling and bony cortical thickening post febrile illness Xrays; periosteal reaction, ulnar/jaw Diff diag; child abuse, hypervitaminosis A, infection, scurvy Prognosis; Benign, self limiting Connective tissue syndromes Marfan Syndrome Pathology; Autosomal Dominant, disorder of alpha 1 unit of collagen synthesis Clinical findings; Arachnodactyly, pectus deformities, scoliosis, spondylolisthesis, heartvalve abnormalities, superior lens dislocation. Joint laxity, protrusio acetabuli Management; Joint laxity, conservatively, scoliosis and spondo. aggressively with surgery.Protrusio acetabuli with triradiate cartilage fusion Ehlos Danlos Syndrome Pathology; Autosomal Dominant, , skin laxity, joint hypermobility vascular fragility Types; 11 types, , types 11 and 111 most common, least disabling Treatment; Physio, orthotics, soft tissue procedures fail Homocystinuria Pathology; Investigations; Autosomal recessive, inborn error of methionone metab. Accumulation of homocysteine Osteoporosis, marfanoid habitus, but with stiffening, inferior lens dislocation. CNS effects Increased homocysteine in urine.(cyanide nitroprusside test) Implications; Treatment; Thrombosis ppted by minor procedures. Vit B6 and reduced methionone diet Clinical findings;