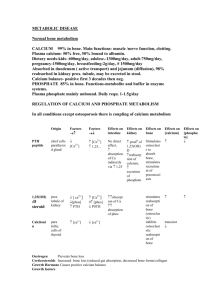
Ca++ and Pi Homeostasis
Ca++ in the plasma
• [Ca++ ] in plasma: 2.5 mM, of which about
½ is bound and thus physiologically
inactive.
• Ratio of free/bound is sensitive to [H+] and
[HPO42-] according to the solubility product
constant
Effector Sites
– Bone (contains 99% of total body Ca++ as
phosphate salt)
– GI tract (mediates uptake from diet, but also
carries out some secretion)
– Kidney (loss/conservation of plasma Ca++
and phosphate)
Regulatory hormones
• Parathormone from parathyroids – 4
(usually) located (usually) on ventral
surface of thyroid
• 1,25 diOH cholecalciferol (1,25 diOH D)
• Calcitonin from thyroid
Parathormone (PTH)
• secretion stimulated by drop in plasma
free Ca++ activity – not total plasma Ca++ protects plasma free Ca++
• Effects:
– increased bone breakdown (osteoclasts)
– Increased activation of “Vitamin” D
– Increased renal Ca++ recovery (connecting
tubule segment of DT)
– Decreased renal phosphate reabsorption
“Vitamin” D (1,25 diOH Cholecalciferol)
Synthesis:
UV light
(Diet, liver synthesis)
7-dehydrocholesterol
PO4
PTH
Kidney - 24hydroxylase
(Liver - 25hydroxylase)
(Skin)
Vit D3
12-OH CC
Kidney – 1hydroxylase
PTH
PO4
24,25-diOH CC
(inactive)
1,25 diOH CC (active)
1,25-diOH CC effects
• Increased Ca++ uptake in intestine (direct)
• Increased bone mineralization (indirect – the
result of uptake stimulation)
• Increased bone breakdown (direct, like PTH)
• Estrogen and testosterone have similar effects;
corticosteroids have antagonistic effects
• Vit. D is necessary for bone growth, but can
channel dietary Ca++ into plasma or bone
depending on the levels of PTH.
Calcitonin
• Secreted by thyroid
• Inhibits bone breakdown
• Role in Ca++ homeostasis in humans is
apparently minor, but it is used as a drug
against osteoporosis – must be injected or
applied as a nasal mist.
Fate Map of Ca++ in the body
BONE (1 kg)
280
mg/d
calcitonin
PTH, corticosteroid
1,25 diOH CC
Diet
1,000mg/d
PLASMA
PTH
1,25 diOH CC
INTESTINE
500 mg/d
325 mg/d
FECES
825 mg/d
9,825 mg/d
KIDNEY
10,000
mg/d
175 mg/d
URINE
Coordinated responses in calcium
homeostasis
How about phosphate regulation?
Remember that decreasing plasma
phosphate will increase plasma free
calcium
Short-term effects of disorders of
Ca++ regulation
• Hypocalcemia: increased excitability of
nerve and muscle with characteristic
muscle spasms and contractures and
cardiac arrhythmias – CNS agitation– “grass tetany” in grazing animals that feed on
low Ca++/high Mg++ diet
• Hypercalcemia: depressed excitability of
excitable cells – lethargy, memory loss
– PTH-secreting parathyroid tumors
Long-term effects of homeostatic
failure
• Vit. D deficiency or dietary Ca++ deficiency
– Rickets – malformed bone in children
– Osteomalacia – adult rickets
• Lack of sex steroids after puberty, or
treatment with corticosteroids
– osteoporosis – loss of bone mass, without
morphological abnormality
What you need to know about K+ regulation
• Plasma [K+] = 4 mEq/l
• Dietary K+ partitioned mainly into intracellular
compartment
• Kidney filters K+, essentially all of the filtered load is
reabsorbed in the PCT
• But then, some K+ is secreted in the DCT at rates
determined by 2 factors:
– Aldosterone levels, which are responsive to plasma [K+]
– Plasma [H+ ], because the DCT secretes a mix of H+ and K+ to
maintain charge balance against Na+ absorption, and the
secreted ions compete with one another