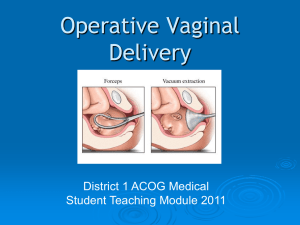
Operative Vaginal Delivery Template
advertisement
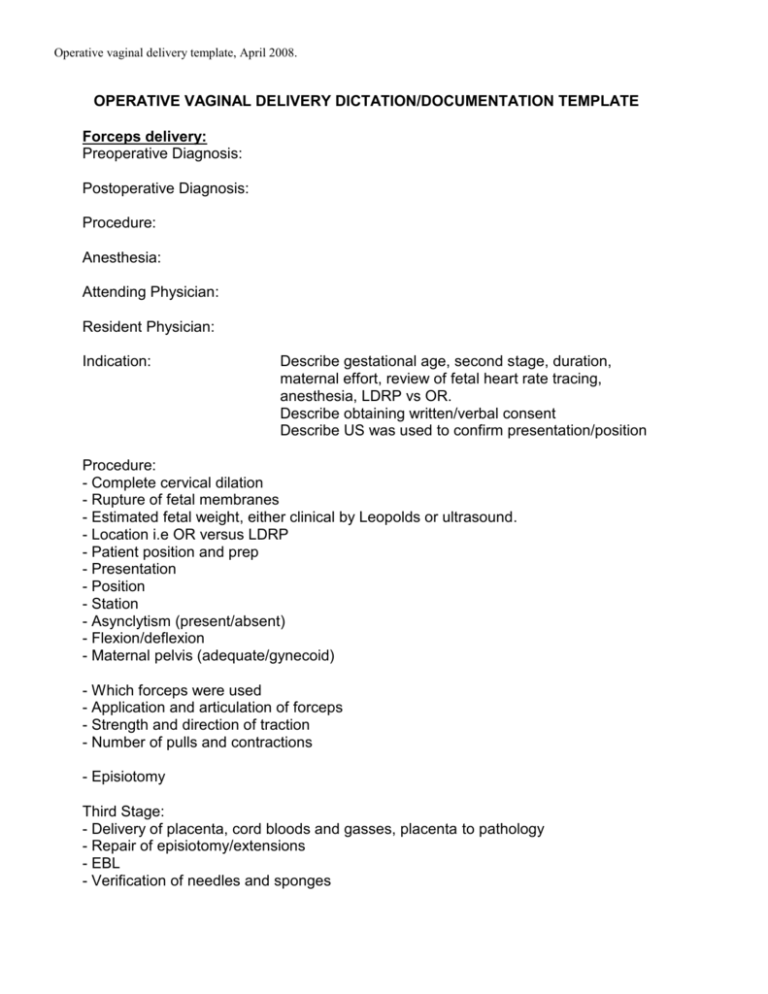
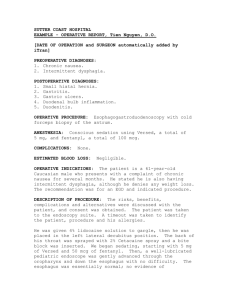
Operative vaginal delivery template, April 2008. OPERATIVE VAGINAL DELIVERY DICTATION/DOCUMENTATION TEMPLATE Forceps delivery: Preoperative Diagnosis: Postoperative Diagnosis: Procedure: Anesthesia: Attending Physician: Resident Physician: Indication: Describe gestational age, second stage, duration, maternal effort, review of fetal heart rate tracing, anesthesia, LDRP vs OR. Describe obtaining written/verbal consent Describe US was used to confirm presentation/position Procedure: - Complete cervical dilation - Rupture of fetal membranes - Estimated fetal weight, either clinical by Leopolds or ultrasound. - Location i.e OR versus LDRP - Patient position and prep - Presentation - Position - Station - Asynclytism (present/absent) - Flexion/deflexion - Maternal pelvis (adequate/gynecoid) - Which forceps were used - Application and articulation of forceps - Strength and direction of traction - Number of pulls and contractions - Episiotomy Third Stage: - Delivery of placenta, cord bloods and gasses, placenta to pathology - Repair of episiotomy/extensions - EBL - Verification of needles and sponges Operative vaginal delivery template, April 2008. Describe neonatal resuscitation and findings; - Apgar scores - Forceps marks - Presence/absence of bruising - Facial symmetry Vacuum delivery: Describe which type of vacuum was used (Kiwi, Mityvac or Mystic) Describe number of pulls (maximum 4) Describe vacuum pressure in between pulls/contractions Describe number of "pop offs" (maximum of 3) Operative vaginal delivery template, April 2008. Example of Forceps delivery: Preoperative Diagnosis: Arrest of descent, 3 hour second stage Postoperative Diagnosis: Arrest of descent, low forceps delivery, right medio-lateral episiotomy. Procedure: Low forceps delivery, right medio-lateral episiotomy. Anesthesia: Epidural Attending Physician: Resident Physician: Indication: Ms. Johnson is a 32 yr. old, G1P0, estimated gestational age 40 2/7 weeks. Labor course was uneventful; however arrest of second stage was diagnosed after 3 hours and 10 minutes of pushing. Fetal heart rate strip was reviewed and assessed as reassuring. Patient had adequate epidural anesthesia. The cervix had been completely dilated and the fetal membranes had been ruptured. The estimated fetal weight was 8lbs. Patient and husband were informed of the diagnosis and a low forceps operative vaginal delivery recommended. Alternatives including Cesarean Section and procedure associated risks were reviewed. Written consent was obtained. Procedure: The patient was transferred to OR A, and transferred to the OR table. Patient was placed in a dorsal lithotomy position and prepped and draped in a routine sterile fashion. The infant was in the vertex presentation, left occiput anterior position, +3 station. There was no evidence of asynclytism, the fetal head was well flexed. The maternal pelvis was felt to be adequate and of the gynecoid type. The presentation and the position of the infant were confirmed by ultrasound. Simpson Luikart forceps were applied without difficulty and articulated easily. Using downward moderate traction, during one set of contractions, the infant was delivered over a right medial lateral episiotomy without difficulty. Operative vaginal delivery template, April 2008. Mouth and nares were suctioned after which the remainder of the infant was delivered, cord was clamped and cut and the infant handed over to the pediatric care providers. Cord blood and cord gases were obtained after which the placenta was removed by gentle traction and sent to pathology. The vagina was inspected and a left succus tear was noted. The right medio-lateral episiotomy was evaluated and did not reveal any extensions. The sulcus tear as well as the medial lateral episiotomy were repaired in the usual fashion using 3-O Vicryl suture. Excellent closure was accomplished. Estimated blood loss during the procedure was 400cc. Sponge and needle counts were correct at completion of the procedure. Apgar scores were 8 and 9. There were minimal marks on the babies head from the forceps. Facial exam was Symmetric and no bruising was noted.