Chapter 6 - wcunurs206and216
advertisement

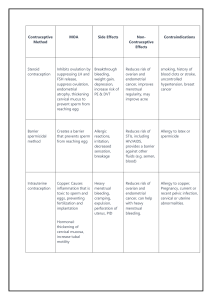
Gloria Nwagwu MSN, FNP-BC, RN Assessment ◦ Establishing trust ◦ Obtaining the sexual history Nursing diagnosis Planning and implementation of care Evaluation Providing Contraception Care Methods of Contraception Natural family planning Fertility awareness Coitus interruptus Lactational amenorrhea method (breastfeeding) Abstinence—0% failure rate Inexpensive Protect against STIs Must be used prior to intercourse Water-based lubricant Few side effects Key: consistent and correct use Diaphragm Cervical cap Condoms (male and female) ◦ Latex allergies Spermicides Contraceptive sponge Oral contraceptives ◦ Monophasic, biphasic, triphasic ◦ Warning signs: ACHES Low-dose progestin-only Transdermal contraceptive patch Vaginal contraceptive ring Initial examination 3-month follow-up after beginning OCPs Yearly examination Regulate menstrual bleeding Mediate menopausal symptoms ◦ Hot flashes ◦ Vaginal dryness Smoking and age greater than 35 years Moderate/severe hypertension (BP 160/100) Undiagnosed uterine bleeding Diabetes of more than 20 years’ duration or with vascular complications ◦ History of pulmonary embolism or deep venous thrombosis ◦ ◦ ◦ ◦ Headaches Breakthrough bleeding Nausea Breast tenderness Cyclic weight gain Hormonal methods (two FDA-approved) ◦ Preven ◦ Plan B Copper-releasing intrauterine device Depo-Provera ◦ Injected every 3 months ◦ Reversible after 10 months ◦ Side effects: irregular bleeding, weight gain, depression ◦ Safe for breastfeeding mothers Implanon ◦ Single rod ◦ Effective for 3 years ◦ Side effects: bleeding irregularities, emotional lability, depression, weight gain Warning signs: PAINS Benefits: ◦ ◦ ◦ ◦ No continued expense No daily attention No interference with intercourse May decrease risk of endometrial cancer Side effects Contraindications ◦ Irregular bleeding ◦ Amenorrhea ◦ Pelvic infections ◦ Current STI ◦ Genital tract cancer ◦ Uterine anomalies, fibroids Female ◦ Bilateral tubal ligation ◦ Nonincisional hysteroscopic tubal ligation Male ◦ Vasectomy Ends pregnancy before fetus reaches age of viability (20 to 24 weeks) 1973—Roe v. Wade Elective abortion Therapeutic abortion Guidance—pregnancy testing, ultrasonography Emotional support Counseling—options, potential complications Information about contraception Menstrual extraction, endometrial aspiration ◦ 5 to 7 weeks gestation ◦ No anesthesia Vacuum aspiration ◦ Up to 12 weeks gestation ◦ Laminaria for cervical dilation Between 8 and 12 weeks of gestation ◦ Mechanical dilation of cervix ◦ Local anesthetic ◦ Complications: uterine perforation, cervical lacerations, hemorrhage, infection, and adverse reactions to the anesthetic agent Second trimester ◦ Cervical dilation and uterine evacuation ◦ Laminaria—24 hours preprocedure ◦ Possible long-term adverse effects from cervical trauma Assessment Emotional support Observe for complications ◦ Excessive bleeding and cramping Schedule follow-up appointment Up to 63 days of gestation Medications induce uterine contractions Mifepristone (Mifeprex, RU-486) Methotrexate Misoprostol (Cytotec) Several days after medication—painless, heavy bleeding, expulsion of tissue Encourage friend/relative for emotional and physical support Follow-up visits ◦ Ultrasonography ◦ hCG levels Second trimester ◦ Vaginal or intrauterine prostaglandins ◦ Repeated doses ◦ Side effects: nausea, vomiting, diarrhea, cramping ◦ Intrauterine hypertonic solutions (rare) Cramping, bleeding Rare: infection, incomplete abortion, hemorrhage, Asherman syndrome, postabortal syndrome Nurse’s role ◦ Educate regarding signs of short-term complications 1. a. b. c. d. The nurse is planning an educational session about contraception. What is the most significant factor in choosing a specific method of contraception in order to avoid pregnancy? Absolute reliability Ease of use Consistency of use Cost 2. When teaching a woman about the use of the diaphragm, it is important to instruct her that the diaphragm should be rechecked for correct size a. Every five years b. When weight gain or loss beyond five pounds has occurred c. After each term pregnancy d. Only after significant weight loss 3. Which of the following is an absolute contraindication to the use of OCP? a. Smokes b. Using antibiotics for UTI c. History of miscarriages d. Gestational diabetes The Nurse’s Role in Infertility Care Sterility Infertility Nurse’s role ◦ Educate—overview of infertility evaluation, basal body temperature ◦ Counseling ◦ Assess understanding of fertile times Female ◦ ◦ ◦ ◦ ◦ Thyroid function test Glucose tolerance test Serum prolactin levels Specific hormonal assays Ultrasonography Female (cont’d) Male ◦ Endometrial biopsy ◦ Hysterosalpingography ◦ Laparoscopy ◦ Semen analysis ◦ Additional tests (endocrine, postcoital test, ultrasonography) Medications to induce ovulation Surgical options Therapeutic insemination Advanced reproductive technologies Factual information—advantages and limitations Financial implications Donor confidentiality Ongoing education and counseling Emotional stress Feelings of disappointment and failure Sense of loss and grief Intercourse changes to goal-oriented procedure Healthy lifestyle choices ◦ Physical activity, nutrition, stress management, adequate rest Holistic/complementary alternatives Herbal supplements Surrogacy—gestational carrier ◦ Ethical/legal implications Adoption Child-free lifestyle Empowerment Advocacy Education Appropriate care to encompass the cultural, spiritual, and environmental domains An infertile couple confides in the nurse at the infertility clinic that they feel overwhelmed with the decisions that face them. Which of the following nursing strategies would be most appropriate? a. b. c. d. Refer them to a marriage counselor Provide them with information throughout the diagnostic process Express concern and provide advise Inquire about the names they have chosen for their baby