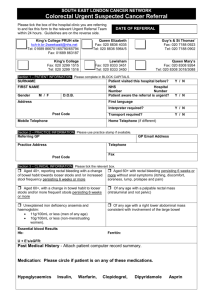
Rectal Bleeding Referral Guidelines for Primary Care
advertisement

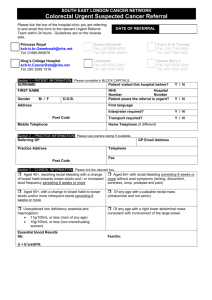
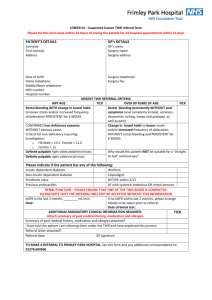
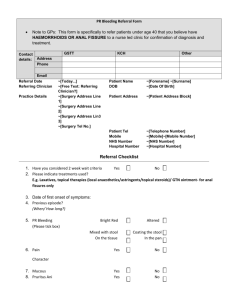
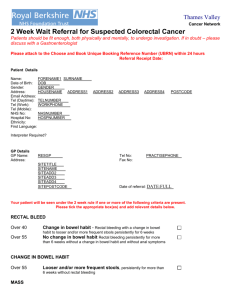
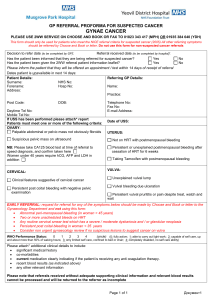
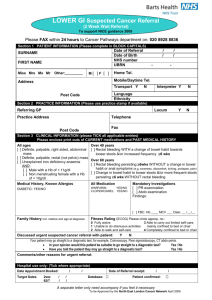
Rectal Bleeding General points Patients with persistent low-risk symptoms which do not respond to treatment, or which recur after stopping treatment, should be referred Please consider the most likely diagnoses and tailor referral urgency accordingly i.e. 2 week wait or urgent or routine thus: 2 week wait criteria Definite palpable right sided abdominal mass probably involving large bowel Definite intraluminal (not pelvic) rectal mass Unexplained iron deficiency anaemia with o Hb < 11g/dl in men o Hb < 10g/dl in non-menstruating women 40-60 yrs old with persistent (>6 weeks) rectal bleeding and a change to looser / more frequent stools 60 yrs or over with persistent (> 6 weeks) rectal bleeding (in absence of anal symptoms) and / or change to looser / more frequent stools Urgent referral – any of: age > 50 at onset, in the absence of anal symptoms blood mixed with stool passage of altered blood or clots associated change to looser stools bleeding in the absence of anal symptoms weight loss strong family history of colorectal cancer - one first degree relative age < 45 or 2 first degree relatives abdominal pain suggestive of partial bowel obstruction iron deficiency anaemia Routine referral for low risk symptoms Persistent symptoms and absence of 2 week wait or urgent criteria above NB: the risk of having bowel cancer is never zero, even in patients without symptoms. Some cancers will be found incidentally in patients presenting with symptoms from benign disease, and symptomatic cancers can develop in patients who already have symptoms from functional bowel disease or piles. This means that patients with persistent low-risk symptoms which do not respond to treatment, or which recur after stopping treatment, should be referred to routine clinics. Page 1 of 2 Investigations prior to referral FBC if anaemic ferritin and CRP Top tips for primary care (once diagnosis confirmed) Haemarrhoids topical treatments with steroid e.g. scheriproct / proctosedyl for a week maximum - see BNF for details Anal fissure rectogesic ointment Diverticular disease milder disease in the younger patients - treat as IBS more severe disease in older patients - low fibre diet and avoid NSAIDs diverticulitis - antibiotics e.g. augmentin and admit if systemically unwell Page 2 of 2