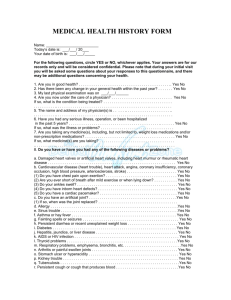
Return Patient Questionnaire
advertisement

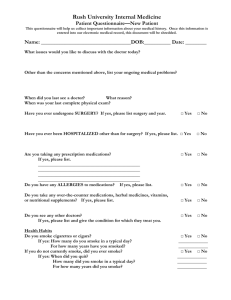
Rush University Internal Medicine Patient Questionnaire—Follow-up visit This questionnaire will help us collect important information about your medical history. Once this information is entered into our electronic medical record, this document will be shredded. Name: _________________________________DOB:___________ Date: _________ Do you have specific concerns you wish your doctor to address? (If yes, please list.) □ Yes □ No Since your last visit, have you been hospitalized or had surgery? If yes, please list. □ Yes □ No Since your last visit, have you been diagnosed with a new medical problem? If yes, please list. □ Yes □ No If taking medications, do you think you are having any side-effects from any of your medications? □ Yes □ No Are you taking any vitamins, herbal preparations, or nutritional supplements? If yes, please list. □ Yes □ No Please list the medical problems for which you are being treated. Please list the medications (with dose and frequency) that you are taking. Please list the names of other physicians, counselors, or therapists who you are currently seeing. Have you undergone any diagnostic testing since your last exam? If yes, please list. Did you receive an influenza vaccination for the current flu season? If yes, please give the date. Have you ever received the pneumococcal vaccine? If yes, give date. □ Yes □ No □ Yes □ No Date: _________ □ Yes □ No Date: _________ When was your last tetanus vaccine? Date: _________ Since your last exam, were you given any other vaccinations? If yes, please list. □ Yes □ No Name: _________________________________ DOB:__________ Date: ________ Please note any changes to your family’s medical history since your last visit. Relative Age (or circle age at death) Medical conditions Natural father Natural mother Paternal: grandfather grandmother Maternal: grandfather grandmother Siblings: Do you smoke? If yes, how many packs per day? Do you drink alcohol? If yes, how many drinks per day? If yes, are you concerned about your level of drinking? Do you ever drink more than 5 drinks in a day? Do you use any other types of drugs? □ Yes □ No ________ □ Yes □ No ________ □ Yes □ No □ Yes □ No □Yes □ No Have there been any significant changes in the following. If yes, please describe the changes. Personal life? □Yes □ No Family life? □Yes □ No Work life? □Yes □ No Screening tests Women: When was your last Pap test? ______ Was it normal? ____________ If you are over age 30, were you tested for HPV? ____________________ If over age 40, when was your last mammogram? ________________________ If you have gone through menopause, when was your last bone density test? Men: If over age 50, or over age 40 with a father or brother with prostate cancer, have you ever been counseled regarding prostate cancer screening? Both: If over age 50, or over age 40 with a parent or sibling with colon cancer, when was your last colonoscopy? ____________________________ When was your last eye exam? __________________________________________ When was your last dental exam? _______________________________________ Name: ___________________________________DOB:_________ Date: _________ Do you exercise? If yes, please describe type and frequency of exercise. □ Yes □ No Review of Systems: Currently, do any of these apply to you? If yes, check box. □ feel at risk for falling Pain (if present, specify where the pain is) □ experienced daily: ____________________ □ experienced infrequently: ______________ Constitutional □ weight loss greater than 10 pounds □ weight gain greater than 10 pounds □ fatigue without effort □ loss of appetite □ persistent fever Head □ headaches □ facial pain Eyes □ failing vision not correctable □ sudden loss, dimming, blurring □ eye pain □ eye redness □ double vision Ears □ difficulty hearing □ recurrent ear infections □ ear injuries □ persistent ringing/buzzing Nose □ inability to smell □ frequent nosebleeds □ persistent congestion/drainage □ difficulty breathing through the nose Mouth □ sores that do not heal □ tooth loss □ change in taste Throat □ frequent sore throats with fever □ hoarse voice without a cold Neck □ lumps or swelling in your neck Breast □ lump in the breast (or under the nipple) □ discharge from or pain in the nipple Cardiovascular □ chest discomfort, pressure, tightness, pain □ shortness of breath with exertion □ awakening at night short of breath □ palpitations (hard or racing heart beat) □ heart murmur □ pain or cramping in legs when walking □ swollen legs Respiratory □ shortness of breath with exertion □ persistent cough □ chronic sputum production □ coughing up blood □ abnormal chest x-ray □ wheezing at rest, with exertion, or at night □ pain in chest with breathing Gastrointestinal □ difficulty swallowing □ frequent or severe heartburn □ frequent or severe abdominal pain □ frequent or new nausea or vomiting □ vomiting blood or black material □ long-standing constipation □ recent-onset constipation □ frequent, loose, or watery stools □ recent change in character of stools □ black or bloody stools □ bleeding from the rectum □ rectal pain Genitourinary □ frequent urination □ burning urination □ urinary infections □ losing control of urine □ bloody, black, or brown urine □ kidney stones women only: □ persistent or severe vaginal discharge □ no menses for more than 6 months unrelated to pregnancy or menopause □ bleeding between menstrual periods □ heavier or more prolonged menses □ bleeding after intercourse □ distressing symptoms related to menses □ losing interest in sex □ hair growth on face, chest, abdomen men only: □ weak or slow urinary stream □ prostate problem □ burning or discharge from penis □ swelling or lumps in the testicles □ pain in the testicles □ losing interest in sex □ unable to attain or sustain erections □ development of abnormal breast tissue Musculoskeletal □ aching muscles □ lasting or repeated back pain □ lasting or repeated neck pain □ painful, swollen, or stiff joints □ painful feet Skin □ persistent skin problem □ skin rash □ dark moles □ change in skin pigmentation □ unusual hair loss □ skin lesion that bleeds or does not heal Neurologic □ dizziness (spinning) □ loss of consciousness □ seizures □ weakness in an arm or leg □ loss of balance while walking □ numbness or tingling in arms or legs □ loss of control of bowels or bladder □ repeated muscle spasms/cramps □ inability to sleep adequately at night □ chronic sleepiness, fatigue, tiredness Psychiatric □ treated for any psychiatric illness □ depressed moods □ diminished interest/pleasure in activities □ difficulty sleeping or sleeping too much □ fatigue/loss of energy □ decreased ability to concentrate □ decreased ability to make decisions □ nervousness, anxiety, irritability □ intense fear or discomfort Endocrine □ elevated blood sugar □ elevated cholesterol □ bone fractures not caused by trauma □ a tendency to always feel hot □ a tendency to always feel cold □ increased thirst all the time □ increased appetite Hematologic □ anemia □ easy bruising □ persistent bleeding from cuts/scratches □ gums that bleed easily if tooth brushing Allergic □ sneezing, chronic runny nose, itchy nose, watery eyes □ persistent coughing not associated with a cold □ cough associated with exercise or exertion □ allergies (dust, mold, ragweed, cats, etc.) If you are ever unconscious following surgery, in an emergency room, or in a hospital, with whom do you authorize us to discuss your case? Does this person have the authority to make decisions for you? Have you completed a Durable Power of Attorney for Health Care? Have you completed a Living Will? Signed: ______________________________________ Date: _______