Colorectal (Lower GI) Referral Form Nov 2014
advertisement

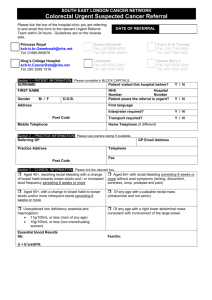
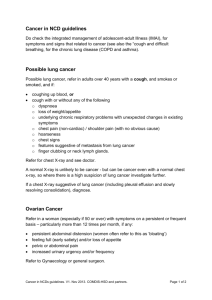
SOUTH EAST LONDON CANCER NETWORK Colorectal Urgent Suspected Cancer Referral Please tick the box of the hospital clinic you are referring to and fax this form to the relevant Urgent Referral Team within 24 hours. Guidelines are on the reverse side. DATE OF REFERRAL King’s College PRUH site kch-tr.br-2weekwait@nhs.net Tel: 01689 866701/65790/65794 Fax: 01689 863187 Queen Elizabeth Fax: 020 8836 4035 Tel: 020 8836 5964/5 Guy’s & St Thomas’ Fax: 020 7188 0923 Tel: 020 7188 0902 King’s College Fax: 020 3299 1515 Tel: 020 3299 1516 Lewisham Fax: 020 8333 3451 Tel: 020 8333 3450 Queen Mary’s Fax: 020 8308 9264 Tel: 020 8308 3018/3088 Section 1 – PATIENT INFORMATION. Please complete in BLOCK CAPITALS. SURNAME Patient visited this hospital before? Y / N FIRST NAME NHS Hospital Number Number Patient aware the referral is urgent? Y / N Gender M / F D.O.B. Address First language Post Code Mobile Telephone Interpreter required? Y / N Transport required? Y / N Home Telephone (if different) Section 2 – PRACTICE INFORMATION. Please use practice stamp if available. Referring GP GP Email Address Practice Address Telephone Fax Post Code Section 3 – CLINICAL INFORMATION. Please tick the relevant box. Aged 40+, reporting rectal bleeding with a change Aged 60+ with rectal bleeding persisting 6 weeks or of bowel habit towards looser stools and /or increased stool frequency persisting 6 weeks or more more without anal symptoms (itching, discomfort, soreness, lump, prolapse and pain) Aged 60+, with a change in bowel habit to looser Of any age with a palpable rectal mass stools and/or more frequent stools persisting 6 weeks or more (intraluminal and not pelvic) Unexplained iron deficiency anaemia and Of any age with a right lower abdominal mass haemoglobin: 11g/100mL or less (men of any age) 10g/100mL or less (non-menstruating women). consistent with involvement of the large bowel Essential blood Results Hb: Ferritin: U + E’s/eGFR: Past Medical History - Attach patient computer record summary. Medication: Please circle if patient is on any of these medications. Hypoglycaemics Insulin, Warfarin, Clopidogrel, Dipyridamole Asprin SOUTH EAST LONDON CANCER NETWORK Information to support Colorectal referrals Refer urgently patients: Aged 40+ reporting rectal bleeding with a change of bowel habit towards looser stools and / or increased stool frequency persisting 6 weeks or more. Aged 60+ with rectal bleeding persisting for 6 weeks or more without anal symptoms. Aged 60+, with a change in bowel habit to looser stools and/or more frequent stools persisting for 6 weeks or more. Of any age with a right lower abdominal mass consistent with involvement of the large bowel. Of any age with a palpable rectal mass (intraluminal and not pelvic). With unexplained iron deficiency anaemia and a haemoglobin of 11g/100mL or below (men) and a haemoglobin of 10g/100mL or below (non-menstruating women). Please check ferritin but do not delay referral. Use this proforma to refer urgently (2 Week Wait) Investigations in Primary Care: Always carry out a digital rectal examination in patients with unexplained symptoms related to the lower gastrointestinal tract. Where symptoms are equivocal a full blood count may help in identifying the possibility of colorectal cancer by demonstrating iron deficiency anaemia, which should then determine if a referral should be made and its urgency. When referring please ensure that the patient has a recent haemoglobin and U + E’s/eGFR as required by NPSA alert “Reducing risk of harm from oral bowel cleansing solutions”. For further information see: http://www.nrls.npsa.nhs.uk/resources/type/alerts/?entryid45=59869&p=2 Faecal occult bloods and tumour markers (e.g. CEA) in symptomatic patients are of little diagnostic value. Low risk symptoms: It is recommended in patients having a normal abdominal and rectal examination and haemoglobin estimation that the following symptoms be used to identify patients at very low risk of bowel cancer: Rectal bleeding with anal symptoms (itching, discomfort, soreness, lump, prolapse and pain). Transient changes in bowel habit, particularly to harder stools and/or decreased frequency of defaecation . Abdominal pain as a single symptom without other high-risk symptoms and signs, an iron deficiency anaemia, or intestinal obstruction. Weight loss in the absence of higher risk symptoms unless rapid and profound. Patients with these symptoms can be initially safely managed in primary care by careful "treat, watchand-wait" strategies and reviewed after 3 months. However, if symptoms persist or recur when off all treatment and Remain low risk – refer routinely to clinic using Choose & Book or a letter. Remain in the low risk category but are worrying / severe – refer to clinic using Choose & Book or a letter, requesting an appointment as soon as possible. Change to higher risk – refer urgently to clinic using this proforma. Risk factors: Offer patients with ulcerative colitis a follow-up plan agreed with a specialist in an effort to detect colorectal cancer in this high-risk group There is insufficient evidence to suggest that a positive family history of colorectal cancer can be used to assist in the decision about referral of a symptomatic patient. Version 3 November 2014 For comments, additional copies, or patient information resources for GPs to use contact the Network on Tel 020 7188 7090 / Fax 020 7188 7120, or visit our website: www.selcn.nhs.uk.