SKIN AND SUBCUTANEOUS
TISSUE
I. Introduction
A. Function
1. Protection
2. Thermoregulation
3. Sensory
B. Anatomy
1. Epidermis – most cellular layer
a. keratinocytes – most numerous
and forms a mechanical barrier
b.Langerhan’s – immunologic
function
c. Melanocytes – pigment
2. Dermis – supporting layer, mostly
fibroblast which produce collagen
3. Basement layer – dermal epidermal
junction
- first layer where blood vessel and
lymphatics are present
- if lesion has not crossed this layer, it
called an “in-situ” lesion
is
II. Pathology
A. Trauma
1. Dirty and infected wounds –
debridement and closed by secondary
intention
2. Lacerations – closed primarily
LACERATIONS
B. Decubitus Ulcer or Pressure Ulcer
- excessive, unrelieved pressure (60 cm
Hg applied for 1 hour)
- muscle more sensitive than skin to
ischemia
- Tx. – debridement and grafting
DECUBITUS ULCER
C. Keloid and Hypetrophic Scar
- over abundance of deposition of collagen
1. Hypertrophic scar – nodularity remains within the
incision
- no treatment necessary
2. Keloid – nodularity goes beyond the incision
- seen more in children and across sternum
- treated with triamcinolone
KELOID
D. Infections
1. Folliculitis – infected
hair follicle
- caused by Staph. sp.
- leads to furuncle
carbuncle
- Tx. – incision and
drainage and
antibiotics
2. Hidradenitis suppuritiva
- plugged apocrine gland
in axilla and inguinal
area
- Tx. – warm compress,
hygiene, discontinuation
of deodorants, open
drainage if recurrent
3. Pilonidal disease – infected
pilosebaceous cysts in the
saccrococygeal area, lined by
granulation tissue
- Tx. – drainage, currete
4. Staphyloccocal Scalded Skin Syndrome
- erythema, bullae formation, loss of
epidermis
- caused by exotoxin from staphyloccocal
infection
- similar to partial thickness burn
-cleavage is in the granular layer
- Tx. – replace fluid, electrolytes, skin care,
antibiotics
STAPHYLOCOCCAL SCALDED SKIN
SYNDROME
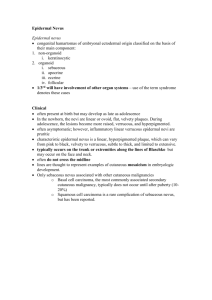
5. Toxic Epidermal Necrolysis
- Immunologic reaction to
certain drugs
such as
sulfonamides, phenytoin,
barbituates, and tetracycline
- Tx. – same as SSSS
6. Viral – verruca vulgaris,
associated with pappiloma virus
- associated with squamous cell
ca
- Tx. – chemical, electrocautery,
surgery
E. Benign Tumors
Cysts
1. epidermal –
sebaceous cysts,
most common
2. Trichilemmal –
occurs
more
commonly in females
3. Dermoid – results
from epithelium
trapped during
midline closure in
fetal development
- Tx. - excision
F. Nevi
1. Acquired
a. Junctional – epidermis
b. Compound – migrates partially
down to the dermis
c. Dermal – cells at dermal layer
- involutes
ACQUIRED NEVI
2. Congenital – rare
- large and may contain hair
- occurs in bathing trunks distribution
- Tx. - excision
CONGENITAL NEVI
G. Vascular
1. Hemangioma
a. capillary
(strawberry)
- compressible, vascular
lesion with sharp borders
- located mostly in the
face, scalp, and shoulder
- observe, 90% involute
b. Cavernous
- bright red or purple, with spongy
consistency
- Tx. – excision
2. Vascular malformation
- enlarged vascular spaces lined with non
proliferating endothelial cells
a. portwine stain – capillary malformation
- Tx. – embolization
b. glomus tumor – painful blue –gray nodules
- arises from the glomus body or SucquetHoyer canal found in the dermis and
contributes to thermal regulation
- may lead to glomangiosarcoma
- Tx. - excision
GLOMUS TUMOR
H. Soft Tissue Tumors
( achrocordons,
lipomas,
dermatofibromas)
- Tx. – excision
I. Neural
- Neurofibromas
(café-au-lait spots)
- associated with von
Reklinghausen’s
disease
J. Malignant Tumors
1. Epidemiology
a. malignant radiation
b. chemicals
c. viral
d. chronic irritation
e. immunosuppresion
2. Types
a. basal cell carcinoma
- most common
- slow growing, rare metastases
- excision with 2-4 mm margin
BASAL CELL CARCINOM
b. squamous cell carcinoma
- metastasizes faster
- Bowen’s disease – ca-in-situ
- Erythroplasia of Queyrat – ca of
the penis
- lesion more than 1 cm has 50%
chance of metastasis
- Tx. – excision with 1 cm margin
- Moh’s technique – serial excision to
preserve skin
SQUAMOUS CELL CARCINOMA
ERYTHROPLASI OF QUEYRAT
c. malignant melanoma
- arises from dysplastic
melanocytes
i. superficial spreading
- most common (70%)
- flat with areas of regression
ii. nodular – 15-20%
- dark, slightly raised
- growth more vertical than
radial
iii. lentigo malignant 5-10%
- best prognosis
- occurs in areas of high solar
degeneration
MELANOMA
b. prognostication
i. Clark
ii. Breslow
iii other factors
- anatomic location –
extremities better than trunk
or face
- ulceration
- inflammatory infitrates
- sex
- histologic type
c. treatment
- still primarily surgical
i. in-situ - .5 to 1 cm margin
ii. T1 (smaller than .76 mm)
- 1-2 cm
iii. thicker lesion – 3 cm margin
- excision is up to the deep fascia
- chemotherapy
- palpable nodes are removed by regional
dissection