Introduction to imaging modalities and main utilities
advertisement

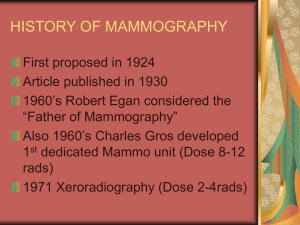
Introduction to imaging modalities and main utilities. Aim and Objectives At the end of the lecture the student should be able to: Define indications for radiological imaging Know different modalities Know the principles of each modality Know the utility of each modality Lecture outline Definition: Radiology is the branch or specialty of medicine that deals with the study and application of imaging technology like x-ray and radiation to diagnosing and Treating disease. Importance of Radiological imaging: It helps in Visualizing the living morphology and function Radiology imaging is a powerful first-line diagnostic tool that is used to identify prenatal congenital abnormalities. Diagnostic radiology , the purpose is to detect and diagnose disease. Interventional radiology, imaging procedures are combined with other techniques to treat certain diseases and abnormalities. Indications: Diagnosing the cause of symptoms and signs. Antenatal evaluation of fetus. Medico-legal (documentation of injury, age determination) Screening. Fitness. Modalities Morphological Imaging : X-rays-radiography Fluorography Computed tomography (CT) scan Mammography Ultrasound waves- sonography Magnetic fields of free H+- magnetic resonance imaging (MRI scan) Positron emission tomography (PET). Functional Imaging Gamma rays –radionuclide scans. X- Ray related Modalities Plain X – Ray. Fluoroscopy. CT Scan Mammography Angiography. Principal of x- ray imaging Most common radiological procedure Made up of still pictures of various organs and tissues in the body X-rays are passed through body to expose photographic film that is placed on the opposite side of body. Changes in film density that result from exposure allows radiologist to distinguish between normal and abnormal tissue and to diagnose many different disease types. Controlled emission of x-rays 2-D, X-D, cross-sections, multi-planar images can be formed Equipment Consists of a large, flat table with a drawer that holds an x-ray film cassette into which a film is placed. Suspended above the table is an apparatus that holds the x-ray tube which can be moved over the body to direct the x-ray Procedure of Plain X – Ray In Film - Screen radiography an x-ray tube generates a beam of x-rays aimed at the patient X-rays passing through patient are filtered to reduce scatter and noise and then strike an undeveloped film, held tight to a screen of light emitting phosphors in a light-tight cassette The film is then developed chemically and an image appears on the film Now replacing Film-Screen radiography is Digital Radiography, DR, in which x-rays strike a plate of sensors which then converts the signals generated into digital information and an image on computer screen Utilities- plain x-rays Best for limbs, chest, abdomen trauma, tumor, infection , inflammation, bone age Used to determine the age using epiphyses. Benefits No radiation remains in a patient's body after an x-ray examination. X-rays usually have no side effects in the diagnostic range. X-ray equipment is widely available in emergency rooms, physician offices, ambulatory care centers, nursing homes and other locations, making it convenient for both patients and physicians. particularly useful in emergency diagnosis and treatment as it is fast and easy. Risks very small risk of cancer from radiation Women should always if there is any possibility that they are pregnant. Fluoroscopy real-time moving images of the internal structures Procedure Consists of an x-ray source and fluorescent screen between which a patient is placed. Modern fluoroscopes couple the screen to an x-ray image intensifier and CCD video camera allowing the images to be recorded and played on a monitor. Fluoroscopy Equipment Risks Radiation doses depend on the size of the patient and length of the procedure Typical skin dose rates quoted as 20–50 mGy/min. Exposure times vary depending on the procedure being performed Due to long length of some procedures, risks include cancer-inducing stochastic radiation effects, deterministic radiation effects eg mild erythema to more serious burns. Common procedures using fluoroscopy Barium swallow Used to examine the upper GI (gastrointestinal) tract Contrast medium drank containing barium sulfate Fluoroscopy images while barium is swallowed. Done typically at a rate of 2 or 3 frames per second. Patient is asked to swallow the Barium a number of times, whilst standing in different positions, i.e. AP, oblique and lateral, to assess the 3D structure. It coats the esophagus with a thin layer of the barium enabling its visualization Commonly used with sodium bicarbonate crystals to produce gas As gas is low in density, and the X-rays pass through very easily, they appear as black patches, as opposed to the white produced by relatively-dense barium. It produces a double contrast image, allowing better visualisation of contrasting features within the mucosal layer of the esophagus. Uses include:Achalasia, oesophageal cancer, tracheoesophageal fistula, gastroesophageal reflux disease (GERD/GORD), hiatus hernia , obstruction of esophagus, oesophageal stenosis Barium follow-through Contrast medium drank containing barium sulfate. It appears white on x-rays, and shows the outline of the internal lining of the bowel. fluoroscopy images taken as contrast moves through intestine, at different time intervals, to enable bowel visulaisation. The test is completed when the barium is visualised in the terminal ileum and caecum, marking beginning of large bowel. Diagnose conditions of the small bowel, eg crohn's disease, ulcerative colitis, bowel cancer Barium enemas Preliminary X-ray is taken to get a baseline image Lubricated enema tube is inserted into rectum The barium contrast medium flows into the colon and monitored via fluoroscopy Colon maybe inflated with air to distend it and provide double-contrast. The patient is moved in different positions to get different views. Thorough cleaning of the large intestine is necessary for accurate pictures. Bowel preparation is necessary before enema procedure. It includes a clear liquid diet, drinking a bottle of magnesium citrate (a laxative), and warm water enemas to evacuate faeces. . Uses include diagnosing and evaluating extent of inflammatory bowel diseases, polys, diverticulitis, interssuspetion, intestinal obstruction. Barium meal Procedure for imaging of oesophagus, stomach and duodenum. The patient ingests gas pellets and citric acid to expand the stomach. Barium sulfate is ingested. The patient may move or roll over to coat the stomach and esophagus in barium and xray taken. Useful in the diagnosis of structural and motiliy abnormalities Two varieties of barium meal: o A single contrast meal uses only barium, o A double contrast meal uses barium as well as a radiolucent contrast medium such as air, nitrogen, carbondioxide. Useful as a diagnostic test, demonstrating mucosal details and allowing the detection of small mucosal lesions eg polyps and diverticuli Angiography Procedure Depending on the type of angiogram, access to the blood vessels via catheter is gained through differeny vessels o Femoral artery for cornoary system o Jugular or femoral vein for right side of heart and venus system Radiolucent contrast agent is inserted in the catheter to visualise blood on the images Types of images X-ray images captured are: o Still images, displayed on a image intensifier or film o Motion images. For most structures, the images are usually taken using a technique called digital subtraction angiography (DSA). o Images usually taken at 2 - 3 frames per second, to evaluate the flow of the blood. o DSA requires the patient to remain motionless, it cannot be used on the heart. Types of angiography Coronary angiography Neuro-vascular angiography Peripheral angiography Computed Tomography An imaging using tomography created by computer processing. Digital geometry processing is used to generate a three-dimensional image of the inside of an object from a large series of two-dimensional X-ray images taken around a single axis of rotation. Process of ‘windowing’ manipulates the data to demonstrate various bodily structures based on their ability to block the X-ray/Röntgen beam. Initially, the images generated were in the axial or transverse plane, modern scanners allow this volume of data to be reformatted in various planes or even as volumetric (3D) representations of structures Equipment The CT scanner is typically a large machine with short tunnel. A narrow examination table slides into and out of the tunnel. Rotating around are x-ray tube and electronic x-ray detectors located opposite each other in a ring, called a gantry. Procedure Positioning on CT examination table according to requirement. Straps and pillows may be used to maintain the correct position If contrast material used, its administered at this stage The table moves quickly through the scanner to determine the correct starting position for the scans. Then, the table will move slowly through the machine as the actual CT scanning is performed. CT scanning of the body is usually completed within 30 minutes. Utility Brain – skull fracture, malformations of the skull, hemorrhage, infract, tumors, CT guided biopsy Chest – CT angiography for pulmonary angiography Abdominal and pelvis - Renal stones, appendicitis, pancreatitis, diverticulitis, abdominal aortic aneurysm, bowel obstruction Extremities - Fractures, ligament injuries, dislocations Benefits Painless, noninvasive and accurate. Can image bone, soft tissue and blood vessels all at the same time. Identifies greater range of densities so best for fat or calcification Can quantify calcium content Very detailed images of many types of tissue as well as the lungs, bones, and blood vessels. Real-time imaging, for guiding minimally invasive procedures eg needle biopsies and needle aspiration of eg lungs, abdomen, pelvis and bones. Diagnosis determined by CT scanning may eliminate the need for exploratory surgery and surgical biopsy. Risks Excessive exposure to radiation may increase risk of cancer. However, the benefit of an accurate diagnosis far outweighs the risk. In general, not recommended for pregnant women unless medically necessary because of potential risk to the baby. Allergic reaction to contrast materials that contain iodine, but is extremely rare Mammography Imaging using a low-dose amplitude-X-rays (usually around 0.7 mSv) to examine breasts A mammography exam, called a mammogram, is used to aid in the early detection and diagnosis of breast diseases Diagnostic as well as a screening tool. Types of images Digital mammography(full-field digital mammography (FFDM)) o X-ray film is replaced by solid-state detectors that convert x-rays into electrical signals. o Electrical signals are used to produce images of the breast that can be seen on a computer screen or printed on special film similar to conventional mammograms. Computer-aided detection (CAD) o Systems use a digitized mammographic image that can be obtained from either a conventional film mammogram or a digitally acquired mammogram. o Computer software highlights abnormal areas of density, mass, or calcification. Equipment Rectangular box containing x-rays tube. Exclusively for breast, with special accessories that allow only the breast to be exposed. Attached to the unit is a device that holds and compresses the breast and positions it so images can be obtained at different angles. Procedure Breast will be placed on a special platform and compressed with a paddle to o Even out the breast thickness so that all of the tissue can be visualized. o Spread out the tissue so that small abnormalities are less likely to be obscured by overlying breast tissue. o Allow the use of a lower x-ray dose since a thinner amount of breast tissue is being imaged. o Hold the breast still in order to minimize blurring of the image caused by motion. o Reduce x-ray scatter to increase sharpness of picture. Change positions between images. The routine views are a top-to-bottom view and an oblique side view. The process will be repeated for the other breast. Utility Screening Mammography Early detection of breast cancer, show changes in the breast up to two years before palpation. Recommend every year, beginning at age 40. Diagnostic mammography To evaluate abnormal clinical finding eg breast lump After an abnormal screening mammography to evaluate the area of concern on the screening exam. Benefits Detect tumour at early stage for early treatment.. Increases the detection of ductal carcinoma in situ (DCIS). Detecting all types of breast cancer, including invasive ductal and invasive lobular cancer. Risks Small risk of cancer from radiation False Positive Mammograms. 5 to15 percent of screening mammograms require more testing such as additional mammograms or ultrasound. Most of these tests turn out to be normal. If there is an abnormal finding, a follow-up or biopsy may have to be performed. False negatives, where small tumours are missed