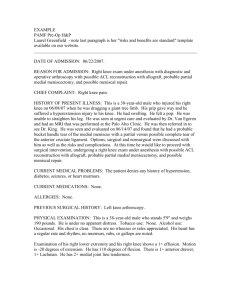
Please read the operative report below and
advertisement

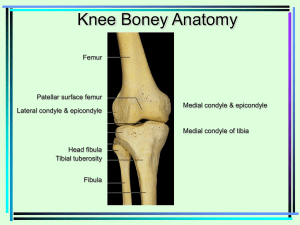
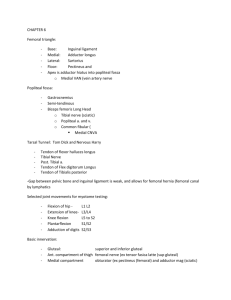
Please read the operative report below and answer the coding/reimbursement questions that follow. OPERATIVE REPORT OPERATION: Examination under anesthesia of the left knee with repair of torn medial meniscus, debridement of posterior horn of lateral meniscus, and patellar tendon/ACL reconstruction, pathology pending. ANESTHESIA: General. PREOPERATIVE DIAGNOSIS: Anterior cruciate ligament-deficient left knee. POSTOPERATIVE DIAGNOSIS: Anterior cruciate ligament-deficient left knee, with associated tears of the medial and lateral menisci, with chondromalacia of the femoral condyles. OPERATIVE FINDINGS: Examination under anesthesia demonstrated a full range of motion from 5-1/2 of hypertension to 145-1/2 of flexion. The knee was stable to varus and valgus stress. It was stable to posterior stress. There was no posterolateral instability. There was a 1+ anterior drawer test, a 2+ Lachman test with a soft end point, and a 4+ lateral pivot shift. At the time of arthroscopy, the patellofemoral joint was unremarkable. The medial femoral condyle, weightbearing surface, had grade 2a, diffuse surface changes with erosion. The weightbearing surface of the lateral femoral condyle demonstrated 2a changes as well, characterized mostly by geographic fissuring throughout. The lateral meniscus had a complex degenerative-type tear involving the entire posterior horn, with cleavage and flap tears about it. After debridement, primarily of the superior leaf of the posterior horn of the lateral meniscus, what was left was smooth, symmetrical, and stable, and measured perhaps 4 mm in thickness. The medial meniscus had an incomplete, but nearly complete, radial tear involving the mid medial portion. The remainder appeared to be intact, although the meniscus itself was soft, if not friable. After repair with a single Innovative meniscus absorbable screw, it was stable. The patellar tendon/ACL graft was secured well to bone. The patella appeared to be isometric, and the graft was not impinged with flexion and extension of the knee. OPERATIVE PROCEDURE: With the 28-year-old patient under satisfactory general anesthesia in the supine position, a systematic examination of the left knee was carried out and the findings have been noted. The left lower extremity was then prepped and draped in the usual manner. Pre-emptive analgesia was supplied with 0.25% Marcaine, 1% Lidocaine, and 2 mg of Duramorph. Two transverse incisions were made: one based at the inferior pole of the patella and the other 4.5 cm distally. These were then used to expose the patellar tendon, where the central third was retrieved as a free bone-tendon-bone ligament graft. The tendon graft was then prepared to pass through a 10 mm sizer. Two #2 Tycron sutures were placed about the tibial bone block and one #1 PDS suture was placed about the patellar bone block. The defect in the patellar tendon was lightly closed with #2-0 Vicryl suture. Next, a systematic arthroscopic evaluation was carried out through anteromedial and anterolateral ports of entry using a Dyonics arthroscope and the findings have been noted. Under arthroscopic control and using an assortment of punches and motorized shavers, the lateral meniscus was derided. Next, using the Innovasive meniscus repair screw, a repair was made on the radial tear of the medial meniscus. Next, a 5-mm notchplasty was performed with a power shaver and motorized bur. The posterolateral outlet of the knee was carefully identified and a Steindler probe marked a spot 6-mm anterior to this outlet at the one o’clock position. Next, a guide pin was placed in the tibia using an Arthrex tibial drill guide. It entered 1 cm medial to the tibial tuberosity and entered the knee joint just anterior to the PCL. Next, the knee was placed in a Stahlberg knee holder at 115-1/2 of flexion. A 3/32nd-inch Steinmann pin was passed through the medial arthroscopy portal into the Steindler spot. This was performed under fluoroscopic control to insure accuracy of location of our femoral tunnel. The Steinmann pin was then advanced out the anterolateral cortex of the femur. A femoral tunnel was then created using serial dilators to an eventual depth of 30 mm and a width of 10 mm. The inner margin of the femoral tunnel was smoothed with a rasp. Next, the tibial tunnel was created using a 10 mm cannulated reamer. The inner margin was smoothed with a rasp and then debrided of soft tissue and cartilaginous tissue with a motorized shaver. The outer margin of the tibial tunnel was debrided of soft tissue. The knee was then placed in 90-1/2 of flexion and a Concept passing pin was passed through the tibial tunnel, the knee joint, and the femoral tunnel, and exited out the anterolateral thigh. This was then used to draw the PDS suture from the patellar tendon graft through the knee joint and thus, under arthroscopic control, the patellar bone block was carefully seated within the femoral tunnel. The knee was then placed back in a Stahlberg knee holder and interference fixation was created in the femoral tunnel using a 7 mm, #20 cannulated Kurosaka screw. The graft was a bit long for interference screw fixation in the tibial tunnel and therefore, an alternative fixation was created by first deepening the distal portion of the tibial tunnel to make it into a trough to receive the bone block. This was then held in place with a small staple, and the Tycron sutures were tied around a post using a #30 AO cancellous screw with a metal washer. There being no further abnormalities, a Hemovac drain was placed in the knee joint and exited out proximal and lateral to the knee. The wounds were then closed using #2-0 Vicryl suture for the subcutaneous tissue and a running subcuticular suture of #3-0 Prolene for the skin incisions. The incisions were reinforced with Steri-Strips, and a sterile dressing was applied. A Bregg ice pack was then applied over a Jobst stocking. The patient tolerated the procedure well, and was discharged from the operating room in satisfactory condition.