patellar tendon moment arms and the screw home mechanism, as
advertisement

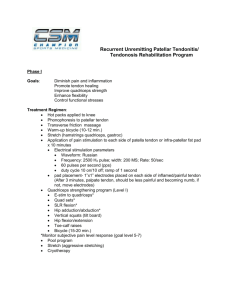
PATELLAR TENDON MOMENT ARMS AND THE SCREW HOME MECHANISM, AS MEASURED NONINVAVSIVELY AND IN VIVO +*?Sheehan, FT; +Rebmann AJ; +?Graham, JM; +SJ Stanhope, SJ +Physical Disabilities Branch, NIH, Bethesda MD; *University of Maryland School of Medicine, Baltimore; ?Catholic University, Washington, DC fsheehan@cc.nih.gov INTRODUCTION The etiology of catastrophic joint tissue failure (e.g., ACL rupture) and systematic wear are believed to be a multi-factorial processes. While activity type, limb positioning, and muscular loading are important contributors, recent utilization of a detailed 3D knee joint model indicates the pivotal role in joint tissue loading played by tibial/femoral/patellar kinematics and patellar tendon forces (1). The moment arm length of the patella tendon relative to the tibial/femoral finite helical axis (FHA) is a key factor in determining joint loading. Yet a clear quantitative in vivo measurement of this important factor is lacking, due to the fact that the majority of previous studies have been 2D, static and cadaver based. A recent study (2) did investigate the patellar tendon moment arm in three dimensions, but was limited to a cadaver model. Thus, the purpose of this study was to experimentally quantify the patellar tendon moment arm non-invasively and in vivo during a volitional leg extension task in healthy volunteers. A secondary goal was to quantify the tibial-femoral FHA in these same subjects in order to determine if the tibia primarily rotates or rotates with translation relative to the femur during extension. The final goal was to determine if the screw home mechanism was evident during this movement. METHODS: Five healthy subjects, [4F/1M, age = 21±1 years, weight = 56.9±2.3 kg, height = 170.7±9.6 m] with no prior history of knee problems or pain participated in this IRB approved study. After obtaining informed consent, subjects were placed supine in a 1.5-T MR imager (LX; GE Medical Systems, Milwaukee, WI, USA). A cushioned wedge, placed under the subject’s thigh, was adjusted so that they could reach full knee extension. Subjects were asked to cyclically extend and flex their knee at 35 cycles/min to the beat of an auditory metronome (2 beats/cycle). Active quadriceps contraction was required to lift the weight of the leg. Prior to data collection, subjects practiced the required task until it could be performed comfortably and consistently. Using a sagittal imaging plane, which was perpendicular to the femoral epicondyles and bisected the patella, a full fast-PC data set was collected (anatomic and x, y, and z velocity images, 24 time frames, temporal resolution = 72 msec, imaging time = 2:48). The imaging parameters were consistent with our prior studies (3). The FHA was defined by the direction of the angular velocity vector of the tibia relative to femur ( and the perpendicular vector connecting the tibial origin to the FHA. was calculated from the 3D fast-PC velocity data. Since the FHA was undefined as approached zero, the FHA was only calculated when 2 <= 0.09 In order to track the tibial and patellar insertions of the patellar tendon, the 3D displacement of points on the patella, femur, and tibia were tracked throughout the motion cycle by integrating the fast-PC velocity data (4). Using rigid body mechanics, the 3D attitudes of each bone were quantified throughout the motion cycle. Figure 2:. Purple line w/circle = t1 (full flex), Purple line w/diamond = t2, … Red line w/diamond = t12 (full ext) RESULTS: All 5 subjects had similar values for the patellar tendon moment arm, which increased in value from max flexion to max extension (Fig 1). In all subjects the FHA shifted posteriorly and slightly inferior relative to the femoral origin (Fig 2). The FHA rotated externally in all subjects during extension. The screw home mechanism was evident (the FHA superior-inferior component was greater than its medial-lateral component) at maximum extension for all subjects reaching a minimum of 6º of knee extension. Subject 5020R did not reach this minimum and demonstrated only slight external rotation. DISCUSSION: To further improve and validate knee joint models and to develop better surgical and rehabilitative protocols for knee joint injury, a complete understanding of subject specific knee joint kinematics and kinetics is required. This study is the first to measure both the 3D patellar tendon moment arm and FHA attitude in vivo during a volitional, weighted task using a completely non-invasive measurement system. One interesting point of note is that the moment arm measured in all 5 subjects increased as the knee extended, opposite to what was reported in a recent 3D cadaver study (2). This increase is consistent with the kinematic data collected in that the FHA tended to shift posterior while the patellar tendon rotated laterally. The discrepancy between these two studies is likely due to the differences in experimental set-up. The study by Krevolin et al (1) was cadaver based with all musculature stripped from the joint and a load applied solely to the quadriceps tendon such that the knee extended at a constant rate. In the current study, the subjects were required to raise their legs against the weight of their own leg, which could account for the posterior shift in the FHA and thus the increasing moment arm. Further, the subjects were free to choose the ratio of force among the four quadriceps muscles and the tensor facia lata remained intact, all of which could account for the external rotation. Work is currently ongoing to complete this same analysis for data collected on over 20 knees. With these data we will be able to investigate if the patellar tendon moment arm is more consistent if normalized and if there are differences in both the FHA attitude and the moment arm based on subject specific parameters. The next step would then be to apply these techniques to the study of specific patient populations. References: (1) Shelburne et al., (2004) J of Biomechanics, 37:797-805 (2) Krevolin et al. (2004) J. of Biomechanics 37:785-788 (3) Rebmann and Sheehan, (2003) JMRI 17 206-213 (4) Sheehan FT et al (2000) Clin Ortho & Rel Research .370 201-207 Figure 1: Moment Arm versus knee angle 51st Annual Meeting of the Orthopaedic Research Society Poster No: 0483