Knee
advertisement

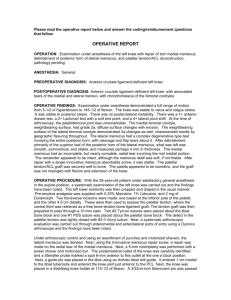
Knee Chapter 16 Anatomy: The knee (hinge) is made of a three articulations: weight-bearing tibiofemoral jt. and the non-weight-bearing patellofemoral jt. Bones: Femur Tibia Patella Because the medial and lateral condyles of the femur differ somewhat in size, shape, and orientation, the tibia rotates laterally on the femur during the last few degrees of extension to produce “locking” of the knee (screwing home mechanism) Menisci: Semilunar (half-moon), functional advantages= absorption and dissipation of force throughout the jt. Medial side is 50% larger than the lateral side, due to the tibia plateau, but the lateral menisci are thicker than medial side. View from above the medial side looks semicircular and lateral looks more circular. Because 74% of total weight of the menisci is water, when the knee undergoes compression during weight bearing much of the fluid is squeezed out into the jt space, providing lubrication to promote gliding of the jt structure. Bursae: Deep bursae, suprapatellar (largest in the body), subpopliteal (lateral condyle of femur/popliteal), semimembranosus (medial head of the gastrocnemius/ semimembranosus tendon), prepatellar (skin/ patella), superficial infrapatellar (skin/patellar tendon), deep infrapatellar (tibial tubercle/ infrapatellar tendon) Ligaments: ACL (Anterior Cruciate Ligament) Tibial attachments, anterior translation PCL (Posterior Cruciate Ligament) Tibial attachments, posterior translation MCL (Medial Collateral Ligament) , Valgus stress LCL (Lateral Collateral Ligament), Varus stress Nerves: Tibial Peroneal Femoral Muscles: Rectus Femoris- Extension Vastus Lateralis- Extension Vastus Intermedius- Extension Vastus Medialis- Extension Semitendinosus- Flexion Semimembranosus- Flexion Biceps Femoris- Flexion Sartorius- Helps w/ Flexion Gracilis- Helps w/ Flexion Popliteus- Helps w/ Flexion Gastrocnemius- Helps w/ Flexion Plantaris- Helps w/ Flexion SOAP’s Notes: History: Same general questions Ask basic questions MOI, when, has it happen before, what did you do for it (Tx), seen by a doctor, etc. Collateral injuries usually results in pain over the injury site. ACL pain is deep or under the kneecap, big pop sound PCL describe as unsteadiness or insecurity over jt line Menisci injuries pain over jt line, with a popping or snapping sound, locking and catching sensation Objective: Look for normal signs (swelling, deformities, eccy, ect.) Genu Valgus (Knock Knees) Genu Varum (Bowlegs) Genu Recurvatum (Hyperextension) Patella Alta (Camel sign) Patella Baja Squinting patella (medial riding) Frog-eyed patella (lateral riding) Injuries Bursitis: Direct blow, overuse, infections, neoplasms (tumors). The prepatellar bursa is injured more frequently by direct blows or shear forces. Swelling may occur immediately or over a 24-hour period. S/S: Swelling, and pain in the bursa region. Management: Ice, compressive wrap, NSAID’s, and avoiding activities that irritate the condition. MCL (Valgus instability): Any lateral force that causes tension on the medial side. S/S: Grade I- mild pain on the jt line, little to no swelling, full ROM w/some discomfort. Grade II- moderate pain, swelling, positive test in 30’ of flexion, unable to fully extend the leg and person may walk on his/her ball of foot. Grade III- pain, no swelling (if swelling is found check the ACL/ Menisci), a positive valgus test w/ a soft end feel or a absent end point. Management: Grade I/II- Ice, compression, rest, immobilizer and crutches (when warrant), NSAID’s, ROM exercises, Grade II- Physician will determine if surgical repair is necessary. LCL (Varus instability): Any medial force that causes tension on the lateral side. S/S: Grade I- mild pain on the jt line, little to no swelling, full ROM w/some discomfort. Grade II- moderate pain, swelling, positive test in 30’ of flexion, unable to fully extend the leg and person may walk on his/her ball of foot. Grade III- pain, no swelling (if swelling is found check the ACL/ Menisci), a positive varus test w/ a soft end feel or a absent end point. Management: Grade I/II- Ice, compression, rest, immobilizer and crutches (when warrant), NSAID’s, ROM exercises, Grade II- Physician will determine if surgical repair is necessary. ACL: Commonly occurs during a cutting or turning maneuver, landing, or sudden deceleration. (ACL injuries are higher in women). S/S: Pain could range from minimal and temporary to severe and lasting. It is described as deep or felt in the anterior on either side of the patellar tendon or laterally on the jt line. 80% of ACL’s people report a popping, snapping or tearing sensation, swelling is rapid (within 3 hrs), weight bearing leads to a feeling of the knee “giving away” or “just does feeling right” Management: Physician will perform surgical repair. PCL: Hyperextension is the most common MOI, but falling on a flex knee w/foot plantar flexed could also cause a PCL tear. S/S: Milder cases, intense pain and a sense of stretching are felt in the posterior aspect of the knee. In total rupture, person reports a pop or snap either heard or felt. Person is aware of swelling, knee extension is limited. Management: Physician will determine if surgical repair is necessary. Meniscal Injuries: Menisci injuries are cause by compression, tensile, and shearing forces. Tears are classified according to age, location, or axis of orientation (Longitudinal/Horizontal= bucket-handle and Parrot-beak). Peak incidence occurs in men between the ages of 21-40 and women 11-20 and 61-70, medial injuries occur more than lateral. Longitudinal tears result from a twisting motion. Horizontal tears results from degeneration. S/S: Meniscal injuries are difficult to assess because 10-30% of the peripheral medial meniscus border and 10-25% of the lateral meniscus border receive direct blood supply. Localized pain, jt line tenderness are the most common findings. Pain occurs on rotation and extreme knee flexion, popping, grinding, or clicking sensation can lead to knee buckling or giving way. Management: Ice, compression, rest, NSAID’s, and crutches when needed. Physician will determine if surgical repair is necessary. Patellofemoral Stress Syndrome: Pain in the patellofemoral joint occurs when either the VMO is weak or the lateral retinaculum that holds the patella firmly to the femoral condyle is excessively tight. S/S: Person reports a dull, aching pain in the anterior knee made worse by squatting, sitting, in a tight space w/knee flexed and descending stairs or slopes. Management: Ice, rest, NSAID’s, strengthening exercises that recruit the VMO muscles. Patellar Tendinitis (Jumper’s Knee): The patellar tendon becomes inflamed and tender from repetitive or eccentric knee extension like running and jumping. S/S: Pain after activity on the inferior pole and insertion of the patellar tendon. As the condition progresses, pain is present at the beginning of activity, subsides during warm-up, then reappears after activity. Eventually, pain is present both during and after activity. Management: Ice, rest, NSAID’s, massage, strengthening exercises. Osgood-Schlatter’s Disease (OSD): This is a traction-type injury to the attachment of the patellar tendon to tibial tubercle. OSD develops in girls between the age of 8 and 13 and in boys between 10 and 15. S/S: Pain at the tibial tubercle and the tubercle appears enlarged and prominent. Pain is w/activity and is relieved w/rest. Management: Self-limiting and takes 12-24 months to run its course. Icing after activities when pain is present, knee padding for sports that involves falling on knees. Sindling-Larsen-Johansson’s Disease (SLJ): Similar to OSD which pain, swelling and tenderness result from excessive strain on the inferior patellar pole at the origin of the patellar tendon. The condition usually is seen in children 8-13 years old. S/S: Pain is gradual and is seen in children involved in running and jumping. Management: Self-limiting and takes 12-24 months to run its course. Icing after activities when pain is present, knee padding for sports that involves falling on knees. Iliotibial Band Friction Syndrome (IT): Common in runners, cyclists, weight lifters and volleyball players. The distal fibers become thicker at their attachment on Gerdy’s tubercle adjacent to the tibial tubercle on the lateral proximal tibia. Individuals with a malalignment problem are predisposed to the condition. S/S: Initially, pain is present only after running a certain mileage (late in run) but as the condition progresses, pain will occur earlier in the run and uphill/downhill/climbing stairs may increase pain. Point tenderness is localized over the lateral femoral condyle. Management: Ice, NSAID’s, and stretching.