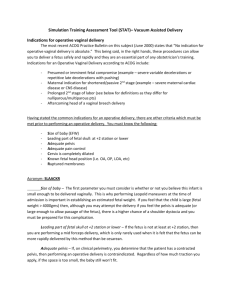
Vacuum Bundle Background and Information (As adapted from Dr
advertisement

Vacuum Bundle Background and Information (As adapted from Dr. Peter Cherouny’s Lecture Series) What causes birth trauma? – Large fetuses – Operative vaginal deliveries (esp midpelvic & combined); Vacuum Assisted deliveries Forceps Deliveries – Vaginal breech delivery – Inappropriate use of pitocin – Abnormal/excessive traction – Inadequate assessment of fetal status What are the risks of vacuum use? To the baby: – Scalp laceration: From 15-40% neonates have cosmetic scalp trauma, related to application time, related to improper placement (off midline), rare long term sequelae – Retinal hemorrhage: Approx 38% of Vacuum instrumented infants, rare long term sequelae – Cephalohematoma: 14-16% of Vacuum instrumented infants, hyperbilirubinemia likely results from blood products reabsorbed after cephalohematoma; most are benign. – Subgaleal hemorrhage: 2.6-4.5% of Vacuum instrumented infants, may be associated with serious long term sequelae and/or death, possibly associated with technique – Intracranial hemorrhage: May be associated with serious long term sequelae and/or death, possibly associated with technique. – Hyperbilirubinemia: Maternal trauma: – Perineal injury – Hematoma formation – Possible association with pelvic floor injury 1 Summary: – Serious complication of Vacuum device in approximately 5% of vacuum attempts – Patients need to be aware of these risks “Given the maternal and fetal risks associated with operative vaginal delivery, it is important that the patient be made aware of the potential complications of the proposed procedure” Operative vaginal delivery. ACOG Technical Bulletin No. 17. June, 2000 Quality Care in Obstetrics Birth Trauma related to Vacuum Delivery Effect of Delivery on Neonatal Injury Method Death ICH SVD 1/5,000 1/1,900 C/S labor 1/1,250 1/952 C/S after OVD 1/333 1/38 C/S no labor 1/1,250 1/2,040 1/105 VD alone 1/3,333 1/860 Forceps alone 1/2,000 1/664 Vacuum and forceps 1/1,666 1/280 Other* 1/216 1/71 1/122 1/76 1/58 *Facial nerve/brachial plexus injury, convulsions, central nervous system depression, mechanical ventilation Towner D, Castro MA, Eby-Wilkens E, Gilbert WM. Effect of mode of delivery in nulliparous women on neonatal intracranial injury. N Engl J Med 1999;341:1709–1714 How we cause birth trauma with the vacuum application – Unnecessary procedure: Prolonged second stage alone is not an indication for immediate delivery, maternal exhaustion can be managed by maternal rest. – High risk procedure: Low chance of success, “trial” of operative vacuum delivery, combination procedure with forceps, gestational age less than 34 weeks. – Inadequate skill of provider: Provider need be credentialed in the procedure, provider must know the definitions of the different types of vacuum delivery, rocking movements should not be used. 2 – Unknown fetal parameters: Estimated fetal weight is critical to the procedural risks, station and position of the fetus must be known, resuscitation team not available. – Prolonged application or multiple pop-offs: Cephalohematoma directly correlated with application time, multiple pop-offs are associated with CPD, fetal injury and failed procedure. – No alternative delivery options available: Cesarean section not readily available, there is a 3-5% unsuccessful rate of delivery, fetal concern often arises during the procedure Vacuum Bundle (5 Bundle Components, recommended 100% review) 1. Alternative labor strategies considered: Including passive descent, resting between pushes, open glottis pushing, avoiding length of second stage parameters if Mom and infant reassuring. 2. Prepared patient Informed consent discussed and documented 3. High probability of success EFW, fetal position and station known 4. Maximum application time and number of pop-offs predetermined Decided upon by the team and supported by manufacturing guidelines and ACOG/AWHONN consensus documents. 5. Exit strategy available Cesarean and resuscitation team available 3