Ankle/ Lower Leg
advertisement
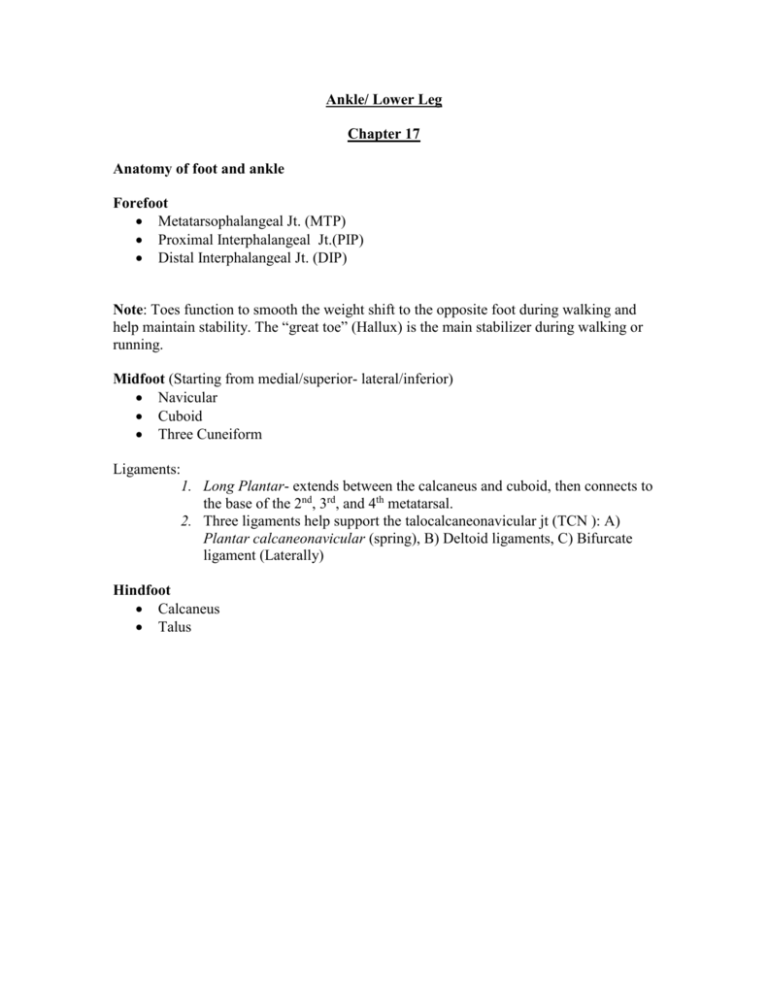
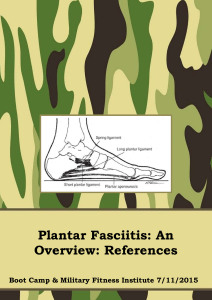
Ankle/ Lower Leg Chapter 17 Anatomy of foot and ankle Forefoot Metatarsophalangeal Jt. (MTP) Proximal Interphalangeal Jt.(PIP) Distal Interphalangeal Jt. (DIP) Note: Toes function to smooth the weight shift to the opposite foot during walking and help maintain stability. The “great toe” (Hallux) is the main stabilizer during walking or running. Midfoot (Starting from medial/superior- lateral/inferior) Navicular Cuboid Three Cuneiform Ligaments: 1. Long Plantar- extends between the calcaneus and cuboid, then connects to the base of the 2nd, 3rd, and 4th metatarsal. 2. Three ligaments help support the talocalcaneonavicular jt (TCN ): A) Plantar calcaneonavicular (spring), B) Deltoid ligaments, C) Bifurcate ligament (Laterally) Hindfoot Calcaneus Talus Talocrural Jt (Ankle) The ankle is modified hinge jt formed by the talus, tibia, and lateral malleolus of the fibula. Fibula assists with weight bearing, supporting approximately 17% of the load on the leg, serves as a site for muscle and ligamentous attachments, and forms the lateral border of the ankle mortise. The ankle capsule is thin and weak, a number of strong ligaments cross the ankle and enhance stability: Deltoid ligaments (medial)- prevents eversion Anterior talofibular ligament (ATFL)- prevents forward motion and inversion during plantar flexion Calcaneofibular ligament (CFL)- prevents inversion Posterior talofibular ligament (PTFL)- strongest of the three and prevents posterior movement. Tibiofibular Jt High Anterior tibiofibular ligament (HATFL) High Posterior tibiofibular ligament (HPTFL) Interosseous membrane Plantar Arches Longitudinal (medially/laterally) - distributes body weight from the talus through the foot, runs from calcaneus to the metatarsals heads. Transverse- distributes body weight from the talus through the foot, runs across the anterior tarsals and metatarsals. Note: Primary supporting structures of the plantar arches: Calcaneonavicular (Spring) ligament, Long Plantar ligament, Plantar fascia (interconnected band of fascia that covers the plantar surface of the foot). Muscles (Four compartments of the lower leg) ROM Anterior: Tibialis anterior (Dorsiflexion) Extensor digitorum longus (Extension) Extensor hallucis longus (Extension) Deep posterior: Tibialis posterior (Plantar Flexion/Inverter) Flexor digitorum longus (Flexion of Toes) Flexor hallucis longus (Flexion of Big Toe) Tibialis posterior artery Tibial nerve Superficial posterior: Gastrocnemius (Plantar Flexion) Soleus (Plantar Flexion) Plantaris (Plantar Flexion) Lateral: Peroneus longus (Eversion) Peroneus brevis (Eversion) Note: Different loading patterns include tension, compression, bending, and torsion. During running foot sustains impact forces two /three times body weight. 50% of body weight is distributed through the subtalar jt to the calcaneus, with remaining 50% through transverse tarsal to forefoot. Toe Deformities Hallus Valgus: Prolonged pressure against the medial aspect of the first MTP jt can lead to thickening of the medial capsule and bursa, resulting in severe valgus deformity of great toe. Hammer Toe: Extended at the MTP, flexed at the PIP, and hyperextended at the DIP Claw Toe: Hyperextension of the MTP, and flexion of the DIP/PIP Mallet Toe: Neutral position at the MTP/PIP, but flexed at the DIP S.O.A.P’s History: (S) Many conditions in the lower leg, ankle, and foot are related to family history, congenital deformities, poor techniques, and recent changes in the training program, surface, or foot attire. Ask basic questions MOI, when, has it happen before, what did you do for it (Tx), seen by a doctor, etc. Changes to distance, duration, or intensity of training. (Overuse injuries) Medial heel pain (Plantar Fasciitis) heel spurs, if in the middle of the plantar heel area. Pain in the medial arch can be a sign of a fallen medial longitudinal arch or tarsal tunnel syndrome. Malleolus pain =ankle sprain. Posterior pain to lateral malleolus = peroneal tendinitis, subluxation, dislocation or sural nerve entrapment. Posterior pain to the medial malleolus = tendinitis, rupture of tibialis posterior. Objective: Swelling, discoloration, deformities, hypertrophy, atrophy, surgical incisions Wear shoes that cause the pain. Deformities, swelling, redness, in the toes, ankle or foot, notice of fallen arch weight-bearing, non-weight bearing. Assessment: Special Testing Injuries Turf Toe: Sprain of the capsular ligament of the 1st MTP, from a hyperextension. S/S: Swelling on the plantar aspect of the MTP jt of the great toe, extension of the great toe is extremely painful. Management: Mild sprains- Ice therapy, nonsteroidal anti-inflammatory drugs (NSAID’s), rest, taping for excessive movement. Moderate to Severe individual may need to be restricted from play. Acute Compartment Syndrome: MOI- Direct blow to the anterolateral aspect of the tibia which may cause a rapid increase space that leads to increased local venous pressure and obstructs the neurovascular network. S/S: Recent Hx of trauma, excessive exercise, a vascular injury, or prolonged externally applied pressure. Management: Ice and total rest. In severe cases ER and surgery. Lateral Ankle Sprains: Acute inversion sprains often occur while changing directions rapidly, also when the foot and ankle is at the moment of loading with plantar flexion and inversion force. S/S: Individual usually reports a cracking or tearing sound. Grade I- Can weight bear immediately after injury, pain, and swelling are mild. Grade II- Swelling and tenderness are localized over the ATFL and may extend over the CFL with some weight bearing. Grade III- Complete tear of one or more of the ligaments. Swelling and ecchymosis are rapid and diffuse functional and clinical instability. Management: Ice therapy, compression, elevation and rest. Crutches for those who cannot weight bear. Syndesmosis Sprain (High Ankle Sprain): Often, the foot dorsiflexed and externally rotated. Rotation causes the ankle mortis to widen. S/S: The point of tenderness is higher, between the tibia and fibula. The ligament that is usually injured is the anterior inferior tibiofibular ligament (AITFL). Management: Ice therapy, compression, elevation and rest. Crutches for those who cannot weight bear. Brace for 3-4 weeks, then a stirrup brace for additional 6 weeks. Strains and Tendinitis: Muscle strains seldom occur in the lower extremity, except in the gastrocnemius-soleus complex. Most injuries occur to the musculotendinous junction or the tendon itself. Most common sites are Achilles tendon, Tibialis posterior, Tibialis anterior, and Peroneal tendon. S/S: Morning stiffness, localized tenderness, possible swelling, pain w/passive stretching and pain w/active and resisted motion. Management: Conservative treatment- Ice, rest, and AROM within levels of pain tolerance. Gastrocnemius Muscle Strain: MOI- Forced dorsiflexion, forced knee extension and muscular fatigue. S/S: Sudden painful tearing sensation in the calf muscle between the musculotendinous junction and the Achilles tendon or in the medial head of the gastrocnemius muscle. Pain, swelling, loss of function and stiffness and later ecchymosis will appear in the foot and ankle. Management: Ice, compression, rest, gentle stretching and strengthening program. Plantar Fasciitis: Most common injury to runners (Extrinsic factors): training errors, improper footwear, and participating in unyielding surfaces. (Intrinsic factors): Pes cavus/ Pes planus, decrease plantar flexion strength, reduced flexibility in the Achilles tendon, and excessive or prolonged pronation and torsional malalignmaents. S/S: Pain on the plantar, medial heel pain that worsens after rest, severe pain in the morning with first steps but diminishes within 5-10 minutes. Pain over the medial side of the calcaneus and increase with passive toe extension. Management: Ice, deep friction massage, ultrasound, electrical stimulation, Achilles tendon stretching and arch strengthening, NSAID’s and soft heel lift. Stress Fractures: Often seen in runners and jumpers particularly after a significant increase in training mileage or a change in surface, intensity, or shoe type. Most common sites: 2nd metatarsal, navicular (jumpers), calcaneus, tibia and fibula (repetitive stress). S/S: Pain during activities and decrease with rest. Management: Rest (4-8 weeks). Avulsion Fractures: Occur at any ligamentous or tendinous attachment. Most common sites: 2nd metatarsal, navicular (jumpers), calcaneus, tibia and fibula (repetitive stress). S/S: Pain during activities and decrease with rest. Management: Rest (4-8 weeks).