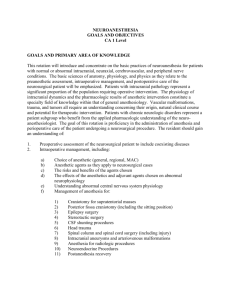
ii. goals & objectives
advertisement
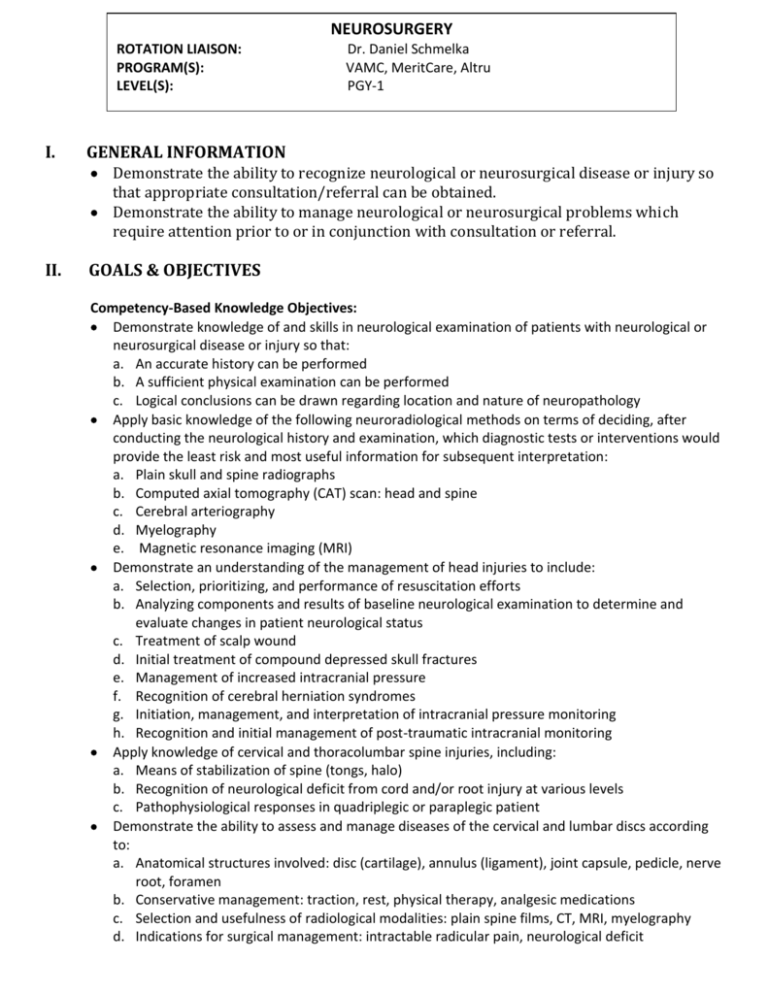
NEUROSURGERY ROTATION LIAISON: PROGRAM(S): LEVEL(S): I. Dr. Daniel Schmelka VAMC, MeritCare, Altru PGY-1 GENERAL INFORMATION Demonstrate the ability to recognize neurological or neurosurgical disease or injury so that appropriate consultation/referral can be obtained. Demonstrate the ability to manage neurological or neurosurgical problems which require attention prior to or in conjunction with consultation or referral. II. GOALS & OBJECTIVES Competency-Based Knowledge Objectives: Demonstrate knowledge of and skills in neurological examination of patients with neurological or neurosurgical disease or injury so that: a. An accurate history can be performed b. A sufficient physical examination can be performed c. Logical conclusions can be drawn regarding location and nature of neuropathology Apply basic knowledge of the following neuroradiological methods on terms of deciding, after conducting the neurological history and examination, which diagnostic tests or interventions would provide the least risk and most useful information for subsequent interpretation: a. Plain skull and spine radiographs b. Computed axial tomography (CAT) scan: head and spine c. Cerebral arteriography d. Myelography e. Magnetic resonance imaging (MRI) Demonstrate an understanding of the management of head injuries to include: a. Selection, prioritizing, and performance of resuscitation efforts b. Analyzing components and results of baseline neurological examination to determine and evaluate changes in patient neurological status c. Treatment of scalp wound d. Initial treatment of compound depressed skull fractures e. Management of increased intracranial pressure f. Recognition of cerebral herniation syndromes g. Initiation, management, and interpretation of intracranial pressure monitoring h. Recognition and initial management of post-traumatic intracranial monitoring Apply knowledge of cervical and thoracolumbar spine injuries, including: a. Means of stabilization of spine (tongs, halo) b. Recognition of neurological deficit from cord and/or root injury at various levels c. Pathophysiological responses in quadriplegic or paraplegic patient Demonstrate the ability to assess and manage diseases of the cervical and lumbar discs according to: a. Anatomical structures involved: disc (cartilage), annulus (ligament), joint capsule, pedicle, nerve root, foramen b. Conservative management: traction, rest, physical therapy, analgesic medications c. Selection and usefulness of radiological modalities: plain spine films, CT, MRI, myelography d. Indications for surgical management: intractable radicular pain, neurological deficit Demonstrate an understanding of important non-surgical problems and post-operative complications relating to neurosurgery, including: a. Closed head injury, problems related to coma, brain swelling, increased intracranial pressure (ICP), ICP monitoring b. Spinal cord injury: problems related to paralysis, sensory deficit, rotobed, tongs, halo c. Airway and respiratory problems secondary to coma or high cord injury: arterial blood gases, respiratory, endotracheal tube, tracheostomy d. Vascular problems: hypo and hypertension, cerebral circulation, cerebral ischemia e. Bladder problems: secondary to brain, cord, or cauda pathology f. Metabolic problems: hypopituitary, hypoadrenal, hyponatremis, water intoxication COMPETENCY-BASED PERFORMANCE OBJECTIVES: Perform neurological history and examination of patients at various levels of consciousness. Write admission, radiological, and preoperative orders under the direction of the supervising attending. Assist during neurosurgical procedures, gaining exposure to and hands-on experience with: a. Bone work: craniotomy, laminectomy b. Neurosurgical hemostasis c. Protection of neural tissues d. Removal of specific lesions: tumor, abscess, hematoma, disc e. Vascular repair: carotid endarterectomy, clipping of aneurysm f. Problems related to cerebrospinal fluid circulation: hydrocephalus Perform limited neurosurgical procedures under direction such as: a. Diagnostic lumbar puncture b. Insertion of ICP monitor c. Repair of scalp lacerations d. Burr hole for subdural hematoma e. Elevation of simple depressed skull fractures f. Application and management of skeletal traction by tongs or halo ACGME CORE COMPETENCIES 1. Patient Care that is compassionate, appropriate, and effective for the treatment of health programs and the promotion of health. Surgical residents must: a. Demonstrate manual dexterity appropriate for their training level, specifically they must be able to first assist on cranial, spinal and peripheral nerve procedures and demonstrate ability for closing surgical wounds on such procedures, assisting during opening and during the main part of the procedures. b. Be able to understand the indications for neurosurgical procedures and demonstrate an ability to identify both surgical and non-surgical options for different disease processes. 2. Medical Knowledge about established and evolving biomedical, clinical, and cognate (e.g., epidemiological and social-behavioral) sciences, as well as the application of knowledge to patient care. Surgical residents should be able to demonstrate medical knowledge pertaining to neurosurgical evaluation and treatment of patients. They are expected to access neurosurgical literature on patients that they see in consultation in the office or hospital and on patients that they assist during surgery. In addition, residents should read or refer to the basic general neurosurgical textbooks including Principles of Neurosurgery by Setti S. Rengachary, MD, Neurological Surgery edited by Youman’s, and Spine Surgery edited by Edward Benzel, MD. 3. Practice-based learning and improvement that involves the investigation and evaluation of care for their patients, the appraisal and assimilation of scientific evidence, and improvements in patient care. Surgical residents are expected to: a. Demonstrate a willingness to learn the basics of principles and practice of neurosurgery as it relates to cranial, spinal and peripheral nerve pathophysiology and should demonstrate a willingness to pursue literature searches of neurosurgical material that is relevant to patients of whom they care for during their rotations. 4. Interpersonal and communication skills that results in the effective exchange of information and collaboration with patients, their families, and other health professionals. Surgical residents: a. Will be an integral member of the neurosurgical team, including the staff physicians, Physician Assistants, Nurse Clinician and the Medical Assistants. b. Are expected to communicate effectively with the Physician Assistants and attending staff regarding patient care. They should be willing to work with the Physician Assistants in the dayto-day patient rounds and hospital-based patient care. c. Are expected to keep track of the type of patients and cases that they are involved with during the rotation so that they can have a broad view of neurosurgery. d. Should communicate with the attending staff during the day previous to a surgical case as to their availability to scrub in on a case. e. Are expected to first assist on neurosurgical cases only if they have reviewed the patient’s case preoperatively and understand the indications for surgery. In addition, residents are expected to meet the patient prior to surgery, preoperatively, either in the office or on the morning of the procedure. 5. Professionalism, as manifested through a commitment to carrying out professional responsibilities, adherence to ethical principles, and sensitivity to patients of diverse backgrounds. Surgical residents are expected to: a. Maintain high standards of ethical behavior. b. Demonstrate a willingness to display continuity of patient care. 6. Systems-based practice, as manifested by actions that demonstrate an awareness of and responsiveness to the large context and system of health care, as well as the ability to call effectively on other resources I the system to provide optimal health care. Surgical residents are expected to: a. Understand the principles of ordering certain radiological and other diagnostic studies and to weigh the cost effectiveness of such studies when making decisions regarding patient care. b. On post-surgical patients, demonstrate and understand the role of different specialists that may be involved in the patient’s care and seeking appropriate consultations in an efficient manner. III. EVALUATION A computerized evaluation will be completed by the faculty at the end of each rotation. Additionally, you are required to submit your evaluation of the rotation and faculty to the residency director. IV. CONTACTS Rotation Liaison – Daniel Schmelka, M.D., Neurosurgery, (701) 780-6283 SCORE CURRICULUM COMPONENTS CATEGORY 28: NERVOUS SYSTEM DISEASES/CONDITIONS BROAD •Management of acute pain FOCUSED •Management of chronic pain OPERATIONS/PROCEDURES ESSENTIAL − UNCOMMON • Digital nerve block COMPLEX •Placement of indwelling epidural catheter •Placement of nerve stimulator for chronic pain •Celiac plexus blockade – percutaneous or endoscopic •Thoracic splanchnicectomy •Peripheral nerve block(s) other than digital 4/21/09; 6/17/10