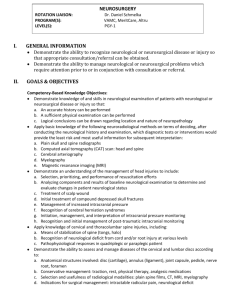
Third Year Rotation Information - Neurosurgery
advertisement
To: UCSD Neurosurgery Third-Year Clerkship Participants I would like to welcome you to the neurosurgical service. We have planned an exciting curriculum that promises to be both exciting and intellectually rewarding. The clerkship will provide an introductory exposure to neurosurgery. In this rotation, you will expand upon your understanding of the basic physiology of the nervous system and explore critical concepts in the pathophysiology of neurosurgical disorders. Didactic sessions have been developed to familiarize you with current research on aspects of neurosurgical treatment. Your participation in patient care provides a fruitful ground for integrating knowledge of the basic neurosciences, disease pathophysiology, and clinical practices. You will be exposed to both inpatient and out-patient neurosurgical practices. Finally, your experiences in the operating room should facilitate an understanding of the basic neurosurgical techniques and etiquette. Mission: A central goal of the clerkship is to provide the students an introduction into neurosurgery as an academic and clinical discipline. The clerkship structure is modeled with emphasis on a problem based approach to learning and emphasis on small tutorial groups – balancing didactics and time for individual intellectual exploration. Specific tutorials are developed to illustrate critical concepts in neurosurgery. The students are asked to actively participate in clinical care of patients as well as first assist in the operating room. The students will also participate in integrative clinical conferences to understand, first hand, how different specialties (e.g. neurology, radiation oncology, and neuroradiology) contribute to defining treatment strategies for patients. General Structure of the Rotation: For the third year rotation, the students will spend the entire month at the Hillcrest site. Operative cases: The students should check in with one of the two chief residents each morning (or preferably the prior evening) in terms of operative case assignment each day. The chief residents will be responsible for optimizing the student’s learning experience. Outpatient clinical experience: Most surgery oriented students necessarily gravitates toward time in the OR. However, it is worthwhile to note that a major portion of learning in surgery lies in when not to operate. In this context, time spent in the outpatient clinic serve as an invaluable learning experience. We strongly recommend that all students participate in the Friday afternoon resident clinic held at the Hillcrest hospital for each of the four weeks of the rotation. Please note that because you will be participating in the brain tumor conference (see below), you will be approximately 45 minutes late for the clinic. The residents will be aware of this scheduling conflict. With the permission of the supervising resident and the attending surgeon, the student may also elect to participate in select attending clinics. Course Material: At the beginning of the rotation, you will be given five hand-outs covering the topics of tumor, vascular, trauma, and spinal neurosurgery. Along with pediatrics and functional neurosurgery, these four areas constitute the major sub-specialties. The course material is meant to give you an over-view of these sub-disciplines. We encourage you to pursue a more in-depth understanding of these topics. Recommended text for this purpose are also enclosed in your orientation package. Teaching sessions: While this is not mandatory, we encourage the students to establish tutorials with as many attending as possible. Please use discretion in terms of balancing operative/clinical learning and tutorials (i.e. don’t let the tutorials be a disruptive force if you are in the middle of a great case). If there are multiple students in a single rotation, the students should organize their time so that all the students are present during the tutorial. The student should expect the session to last 15-30 minutes. The session may take the form of a didactic lecture or in the form of interactive clinical scenarios. Each attending will cover a different aspect of neurosurgery. The topics covered by each attending are as follows: Dr. Barba: functional neurosurgery (DBS) Dr. Chen: Radiosurgery Dr. Nguyen: vascular (AVM) Dr. Khalessi: vascular (ICU management) Dr. Brown: peripheral nerve Dr. Ciacci: spine (trauma) Dr. Carter: tumor (primary) Dr. U: vascular (aneurysms) Dr. Levy: pediatric tumor/vascular Dr. Meltzer: pediatric craniofacial/hydrocephalus Dr. Taylor: spine (degenerative) Dr. Pakbaz: endovascular approaches Dr. Marshall: head trauma Dr. Alksne: functional neurosurgery (trigeminal neuralgia) Calls: For the third year rotation, the over-night call is optional. If the students wish, s/he may contact the resident on call and ask for permission to take over-night call with the resident. If you do take call, you should direct your focus toward how to 1) succinctly summarize pertinent clinical information when presenting cases to attending staff 2) identify resources (both equipment and supervisory expertise) when such resources are generally limited 3) neurosurgical emergencies and the appropriate management. Conferences: The students are expected to participate in the following conferences 1. Friday morning grand round (7:30 AM each Friday morning -- with exception of the month of August. Please note that the grand round may be held at different sites pending on the week. It is the responsibility of the student to check with the Eric Lin, the course coordinator, in terms of the location of the grand round. 2. Teaching conference -- taking place after morning grand round. This conference may take the form of interactive clinical scenario or lecture. 3. Dedicated third year teaching session -- taking after the teaching conference. Each week, the students rotating through the service will meet with me for approximately 30-45 minutes to review key principles in neuro-surgery 4. Neuro-oncology conference -- taking place every week between 11 AM and 1 PM in the Moores Cancer Center Radiation Oncology conference room. Examination: During the last day of the rotation, you will take a written examination instead of attending the neurosurgery clinic. The examination consists of 30 question covering key principles of neuro-radiology, neuro-surgery, neuro-anatomy, neurology, and neuro-anatomy. Evaluation: Your grades will consist of into two equally weighted components. The first component consists of input from faculty and the clinical team in terms of your participation, operative techniques, and general neurosurgery knowledge. The second component consists of your performance on the final examination. As the course director, I will synthesize these components into a formal evaluation that will be submitted to the department of surgery. Exit interview: At the end of the rotation, the student will have an exit interview with me and/or Eric Lin, the course coordinator. While there is a structured exit interview, it is critical that the student let me or any of the faculties know as early as possible when encountering any situation prohibitive to optimal learning. We will do my best to resolve the situation. I know that I speak on behalf of the entire team of faculty, resident, and staff in assuring you that we are committed to your neurosurgical learning. So, please let us know how we can best facilitate your learning. Once again, on behalf of the neurosurgery faculties, residents, and staff members, welcome to the rotation. Sincerely, Clark C. Chen, M.D., Ph.D. Director, Stereotactic and Radiosurgery Co-Director, Surgical Oncology Director, Neurosurgery Clerkship Division of Neurosurgery University of California, San Diego 3855 Health Science Drive #0987 La Jolla 92093-0987 Phone: 619-246-0674 Fax: 858-822-4715 Email: clarkchen@ucsd.edu




![[Date] - Liam`s Fund](http://s3.studylib.net/store/data/007555966_2-920deb421ea4247d1b218128f08ee869-300x300.png)