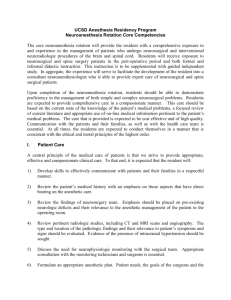
Neuroanesthesia
advertisement

NEUROANESTHESIA GOALS AND OBJECTIVES CA 1 Level GOALS AND PRIMARY AREA OF KNOWLEDGE This rotation will introduce and concentrate on the basic practices of neuroanesthesia for patients with normal or abnormal intracranial, neuraxial, cerebrovascular, and peripheral nerve conditions. The basic sciences of anatomy, physiology, and physics as they relate to the preanesthetic assessment, intraoperative management, and postoperative care of the neurosurgical patient will be emphasized. Patients with intracranial pathology represent a significant proportion of the population requiring operative intervention. The physiology of intracranial dynamics and the pharmacologic results of anesthetic intervention constitute a specialty field of knowledge within that of general anesthesiology. Vascular malformations, trauma, and tumors all require an understanding concerning their origin, natural clinical course and potential for therapeutic intervention. Patients with chronic neurologic disorders represent a patient subgroup who benefit from the applied pharmacologic understanding of the neuroanesthesiologist. The goal of this rotation is proficiency in the administration of anesthesia and perioperative care of the patient undergoing a neurosurgical procedure. The resident should gain an understanding of: 1. 2. Preoperative assessment of the neurosurgical patient to include coexisting diseases Intraoperative management, including: a) b) c) d) e) f) Choice of anesthetic (general, regional, MAC) Anesthetic agents as they apply to neurosurgical cases The risks and benefits of the agents chosen The effects of the anesthetics and adjuvant agents chosen on abnormal neurophysiology Understanding abnormal central nervous system physiology Management of anesthesia for: 1) 2) 3) 4) 5) 6) 7) 8) 9) 10) 11) Craniotomy for supratentorial masses Posterior fossa craniotomy (including the sitting position) Epilepsy surgery Stereotactic surgery CSF shunting procedures Head trauma Spinal column and spinal cord surgery (including injury) Intracranial aneurysms and arteriovenous malformations Anesthesia for radiologic procedures Neuroendocrine Procedures Postanesthesia recovery PATIENT CARE Residents must be able to provide patient care that is compassionate, appropriate, and effective for the treatment of health problems and the promotion of health. Residents are expected to: 1. 2. 3. 4. Perform an appropriate evaluation; including history, physical exam and laboratory studies when needed Interact effectively with patients and their families demonstrating respect and care for individuals. Formulate a plan based on the individual patient’s medical history, expectations and expected course of their condition. Work together with other members of the interdisciplinary health care team, to optimize patient care and enhance quality of life. MEDICAL KNOWLEDGE Residents must demonstrate knowledge about established and evolving biomedical, clinical, and cognate sciences and the application of this knowledge to patient care. Residents are expected to: 1. 2. 3. 4. Apply relevant scientific knowledge and reasoning to the practice of neuroanesthesia. Understand both normal and abnormal central nervous system physiology, neuroanatomy relevant to neurosurgical procedures, cerebral and spinal cord blood volume and flow, the anatomy of the blood brain barrier, the etiology of cerebral edema, the anatomy of peripheral nerves and their innervation, physiology of the NMJ and muscle. Understand neuro-physiological monitoring to include EEG, SSEPS, MEPS, BAEPS, EMG and ICP. Understand the anesthetic ramifications of increased ICP, intracranial masses, intracranial vascular lesions, epilepsy, CSF shunting procedures, head and spine trauma, radiographic procedures, pituitary surgery, peripheral nerve surgery, surgery on patients with muscle disorders, and patients with disorders of muscle INTERPERSONAL/COMMUNICATION SKILLS Residents must be able to demonstrate interpersonal and communication skills that result in effective information exchange and teaming with patients, their patients families, and professional associates. Residents are expected to: 1. 2. 3. 4. 5. 6. Discuss with patients and family members the utility and advantages, as well as potential disadvantages, of the different anesthetic options. Establish good rapport with patients and families, addressing patient and family concerns and anxieties. Create and sustain a therapeutic and ethically sound relationship with patients. Use effective listening skills to elicit appropriate clinical information. Work effectively with others in the interdisciplinary health care team. Establish working relationships with operating room staff, surgeons, resident and 2 attending anesthesiologists. PROFESSIONALISM Residents must demonstrate a commitment to carrying out professional responsibilities, adherence to ethical principles, and sensitivity to a diverse patient population. Residents are expected to: 1. 2. 3. 4. 5. 6. 7. 8. demonstrate respect, compassion, and integrity; a responsiveness to the needs of patients and society that supersedes self-interest; accountability to patients, society, and the profession; and a commitment to excellence and on-going professional development demonstrate a commitment to performing duties as a physician and medical professional. demonstrate a consistent work ethic. demonstrate a consistent level of respect to patients, families, and operating room staff. demonstrate a commitment to ethical principles pertaining to provision of clinical care, confidentiality of patient information, informed consent, and business practices demonstrate sensitivity and responsiveness to patients culture, age, gender and disabilities. demonstrate accountability to patients, colleagues and institution. demonstrate the integrity of a medical professional and a commitment to excellence and ongoing professional development. Residents must be able to investigate and evaluate their patient care practices, appraise and assimilate scientific evidence, and improve their patient care practices. Residents are expected to: 1. 2. 3. 4. locate, appraise, and assimilate evidence from scientific studies related to cardiac and thoracic anesthesia. This includes, but is not limited to, the directed readings in the Core Curriculum. In selected cases, it is appropriate to pursue additional scientific evidence in a reference text or in an electronic online search. be able to synthesize medical information from texts, lectures, and journal articles and apply this information to the care of neuro-surgical patients. apply knowledge of study designs and statistical methods to the appraisal of clinical studies and other information on diagnostic and therapeutic effectiveness use information technology to manage information, access on-line medical information; and support their own education. SYSTEMS-BASED PRACTICE Residents must demonstrate an awareness of and responsiveness to the larger context and system of healthcare and the ability to effectively call on system resources to provide care that is of optimal value. Residents are expected to: 1. understand how their patient care and other professional practices affect other health care professionals, the health care organization, and the larger society and how these elements of the system affect their own practice 3 2. 3. 4. 5. 6. 7. Understand the healthcare system as it relates to neurosurgery and neuro-anesthesiology. The patient preoperative process, diagnosis by neurologists, neurosurgeons, radiologists, through the post op course patients will experience, including ICU, floor care, rehabilitation, and home care. practice anesthesiology within the context of this health care institution and in cooperation with other health care professionals. practice cost-effective health care. advocate for quality patient care and assist patients in dealing with system complexities know how to partner with health care managers and health care providers to assess, coordinate, and improve health care and know how these activities can affect system performance COGNITIVE OBJECTIVES 1. 2. 3. 4. Describe an appropriate anesthetic based on the clinical condition, goals of the procedure, and anticipated intraoperative monitoring for surgeries listed above Describe neuroanatomy relevant to a neurosurgical procedure Understand and explain the physiology of cerebral metabolism, blood flow and blood volume Understand and explain the effects of anesthetic agents and adjuvant drugs on: a) b) c) d) 5. Cerebral metabolism Cerebral and spinal cord blood volume and blood flow Blood brain barrier and cerebral edema Cerebral protection, ischemia and resuscitation Understand the application and the effects of anesthesia on: a) Neurophysiologic monitoring. 1.) 2.) 3.) 4.) 5.) 6.) b) 6. 7. 8. 9. electroencephalography somatosensory evoked responses motor evoked responses peripheral and cranial nerve monitor BAERS EMG intracranial pressure monitoring. Understand and describe the perioperative surgical and anesthetic considerations for fluid management Recognize, understand the origins of, and treatment of intracranial hypertension Interpret and respond to data from monitoring devices (etCO2, CBF, EEG, EMG, SSEP, BAER, ICP) List, and describe ways to avoid, the problems associated with emergence from anesthesia 4 10. 11. 12. 13. 14. 15. 16. Understand CBF and factors affecting it, including CO2 and 02 response and pharmacological changes in CBF. Understand the use of fluids for neuro-surgical patients, including crystalloid, colloid, blood products, mannitol and dextrose-containing solutions. Understand patient positioning and its implications. Understand the pathophysiology of acute and chronic spinal cord injury, including the cardiovascular and pulmonary consequences (especially autonomic hyperreflexia). Understand the consequences of using depolarizing muscle relaxants in these patients. Understand the management of increase ICP for craniotomy and the use, hyperventilation, barbiturate infusion, diuretics and CSF drainage. Have knowledge of airway management and sedation requirements for patients undergoing stereo tactic procedures under GA or local anesthesia. SKILL OBJECTIVES 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. Demonstrate the basic skills of anesthesia to include airway management, starting IVs, Alines, long arm CVP’s, etc. Successfully manage complex neurosurgical cases Utilize multiple anesthetic methods (topicalization, nerve blocks, nebulized local anesthesia) in the preparation of a patient for awake intubations Perform awake fiberoptic intubation and awake positioning with the ability to assess neurologic function as needed Insert, properly interpret, and respond to invasive hemodynamic monitors Perform and properly maintain hypotensive anesthesia when indicated Be able to give a case presentation, including medical problems, pre-anesthesia concerns, airway management, lines, anesthetic medications, and extubation plans in a neurosurgical patient. Be able to review the medical history and physical exam to define the type and severity of the neurosurgical problem, as well as other medical problems the patient may have. Recognize patients with spinal cord pathology and be able to determine which ones may require special techniques (awake intubation) and positioning. Recognize which patients would be appropriate for early extubation (in OR or PACU) considering their CNS, neuromuscular, and other medical conditions. Manage an elective craniotomy and understand the choice for the anesthetic agents. Be able to evaluate CT/MRI images for obvious abnormalities such as epidural and subdural hematomas, large strokes and masses. Manage spine surgery, including cases with potential for massive blood losses. Manage cases in the sitting position. a) b) 17. 18. 19. Pre-cordial Doppler placement - Recognize air entrapment Long-arm CVP placement and management Manage craniotomy for neuroendocrine tumors. Plan an anesthetic to allow for rapid reversal of anesthetic effects to assess neurological function after craniotomy. Be able to place a right atrial catheter for diagnosis and management of air embolism. 5 20. 21. 22. 23. 24. 25. 26. 27. 28. Perform awake laryngoscopy, fiber optic laryngoscopy, fast-track LMA or in-line traction. Understand their use in patients with spinal cord injury. Be able to set up, organize, and execute the planning of a complicated case. Perform preoperative patient assessment and choose an anesthetic plan specific for that neurosurgical patient. Provide the basic skills and experience necessary to care for patients undergoing surgery for intra-cranial masses, intra-cranial vascular surgery, epilepsy, stereo-tactic surgery, CSF shunting procedures, head trauma, radiographic procedures, pituitary surgery, peripheral nerve surgery, surgery on patients with muscle disorders, and anesthesia for patients with disorders of the neuro-muscular junction. Provide appropriate treatment for increased intra-cranial pressure Provide proper fluid management in neurosurgery patients Manage patients with neurologic disease undergoing non-neurosurgery procedures Perform fiber optic intubations, start IV’s, arterial lines, and obtain central venous access Provide initial postoperative care in the ICU/PACU REQUIRED READING Week 1 Cerebral Physiology, Ch 29 Anesthesia, 6th edition, Ronald Miller Ed. Churchill Livingston, 2005 Week 2 Neurosurgical Anesthesia, Ch 53 Anesthesia, 6th edition, Ronald Miller Ed. Churchill Livingston, 2005 Week 3/4 Neurological Monitoring, Ch 38 Anesthesia, 6th edition, Ronald Miller Ed. Churchill Livingston, 2005 EVALUATION Final evaluation will be based upon clinical performance with a written evaluation. Rev. 7/2009 6