Does the use of nebulised adrenaline affect the clinical outcome in
advertisement

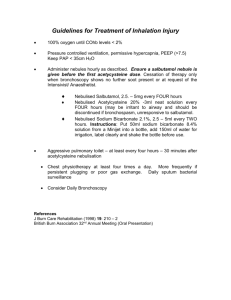
Evidence Based Search Question: Does the use of nebulised adrenaline affect the clinical outcome in infants diagnosed with bronchiolitis? Scenario An 8 month old child presented to CHB with a one day history of dry cough, shortness of breath and fever. There have been no previous similar episodes and no previous hospital admissions, the baby being well and thriving before admission. There is no relative family history and no history of TB contact, with the family living in Soweto in a house with full amenities. The pregnancy was uneventful with the baby born by elective caesarean, weighing 3.100 kg with no complications. The baby was bottle fed from birth, the bottle being sterilized properly and the feeds mixed correctly. The baby was above the 50th centile on the RTHC from birth. On admission the child was in severe respiratory distress with a respiratory rate of 64, intercostal and subcostal recession, alar flaring and oxygen saturation of 93% on nasal prongs. The patient was hyperinflated with extensive wheezing bilaterally but no stridor. There were no other relevant clinical findings. Blood gas analysis showed the patient to be slightly acidotic with a pH of 7.35, pCO 2 of 32.2mmHg and PO2 of 62.2mmHg. Chest X-ray showed hyperinflation with no other findings. An assessment of an acute lower respiratory tract infection, most likely to be a viral bronchiolitis was made. The child was admitted and given nebulised adrenaline and atrovent in saline in a ratio of 1:1:3 and then reassessed. After receiving 2 sets of nebs over 6hours the child was clinically much improved with a respiratory rate of 40, decreased signs of respiratory distress and no wheeze on auscultation. I have often wondered of the need to combine both adrenaline and a beta agonist in the nebulised mixture, so in patients diagnosed with bronchiolitis, mostly due to respiratory syncitial virus does the use of nebulised adrenalin affect flow volume mechanics, clinical course and length of hospital stay, when compared to placebos and other bronchodilators? Search Results 1 Searches were conducted on the Cochrane Database and Pubmed sites, using the keywords “Bronchiolitis” and “Epinephrine”. Cochrane database: 4 articles, 1 relevant. Pubmed: 56 articles, 4 relevant. Commentary Although most of the studies looked at different aspects regarding the outcome of patients treated with nebulised adrenaline, there appear to be conflicting views as to its benefits. However the two Australian studies by Numa A et al and Wainwright C et al both came to the conclusion that there is no indication to treat all patients diagnosed with bronchiolitis with nebulised adrenaline. In fact Wainwright goes on to show that the use of adrenaline in patients needing supplemental oxygen results in a longer hospital stay than those given a placebo. They also found that there was no significant change in hospital stay in those patients not requiring supplemental oxygen in either of the study groups. Their final conclusion was that the evidence they gathered clearly demonstrated that bronchodilators do not produce a clinically relevant improvement in condition or length of stay in hospital. Numa did show that there was a significant change in respiratory mechanics with a decrease in airway resistance, however the majority showed no change in compliance, with more demonstrating a decrease in compliance than those with an improvement. A factor that must be brought in here is that all the patients were intubated and hence there could be no assessment of respiratory effort and any improvement thereof with the administration of adrenaline. Another factor is the size of the study, with only fifteen patients involved. This small population group cannot realistically be thought of as representative of the range of clinical presentations and response to treatment that would normally be seen with bronchiolitis. The study from India firmly concluded that there definitely is a place for the use of bronchodilators in the treatment of bronchiolitis with a significant benefit when comparing adrenaline to salbutamol. Both appeared to reduce respiratory rate, have benefits on respiratory distress 2 assessment and the clinical score, but with adrenaline having a greater effect in all areas. The conclusion of this was that the use of bronchodilators in infants with bronchiolitis was beneficial, with adrenaline being the more efficicacious. Another article that extolled the virtues of the use of bronchodilators was the one from Canada. They showed that there was a significant benefit with the use of bronchodilators in the clinical score and pulmonary mechanics in patients with the first episode of bronchiolitis. They also concluded that the use of adrenaline has superior effects to salbutamol in all aspects of treatment. The only thing against the study was that it had a small study size with a total of 24 patients. As a kind of round-up of the studies there was one relevant article from the Cochrane Database that analysed the results from 14 studies. They found that although there appears to be some benefit in the use of bronchodilators in the treatment of bronchiolitis, namely adrenaline, there is insufficient evidence to support its routine use in in-patients. They do however concede that there is some evidence that adrenaline is more efficacious than salbutamol in out-patient setting. As can be seen from the above articles it still appears that there is a lot of controversy about the use of bronchodilators in children with bronchiolitis. In reviewing these articles I have tried to take into account their strengths and weaknesses. Two of the studies (Numa A and Sanchez I) had small sample sizes which cannot really be taken to be representative of the many different presentations, regarding the degree of respiratory distress in bronchiolitis. It also became clear that most of the studies actually took steps to identify children with chronic lung disorders, which may have contributed to their clinical presentation. Also taking into account the Cochrane Review of the above topic, it would appear that they do not recommend that bronchodilators be given to all patients presenting to hospital with signs of RSV bronchiolitis. In my experience, although the above patient did respond very well to adrenaline and atrovent, I have seen other patients that seem to be no better after receiving 3 sets of nebs with both adrenaline and atrovent. Answer: It would appear that there is benefit in the use of nebulised adrenaline, over the use of salbutamol, and there would appear to be no clinical grounds to deny use of these agents in children with respiratory distress due to bronchiolitis, even if they show no response to treatment. Better to err on the side of safety and treat, as many of the patients will respond, with a possible result of a shorter stay in hospital. A possible course of action would be one suggested in the Lancet; a trial of salbutamol with continuation of treatment in those that respond, with a trial of epinephrine in those that have no response to initial salbutamol therapy. 3 References: 1. Simoes, A., RSV Infection, The Lancet. 1999; 354: 847-52 2. Wainwright, C., et al, Multicentre, Randomised, Double-blind Controlled Trial of Nebulised Epinephrine in Infants with Acute Bronchiolitis, NEJM. 2003; 349: 27-35 3. Numa AH., et al, Effect of Nebulised Epinephrine on Respiratory Mechanics and Gas Exchange in Bronchiolitis, Am J Respira Crit Care Med. 2001; 164: 86-91 4. Singh V., et al, Comparison of Nebulised Adrenaline vs Salbutamol in Wheeze Associated with Respiratory Tract Infection in Infants, Indian Paediatrics. 2002; 39:12-22 5. Sanchez I., et al, Effect of racemic epinephrine and salbutamol on clinical score and respiratory mechanics in infants with bronchiolitis, Journal of Paediatrics. 1993; 122: 145-51 6. Hartling L., at al, Epinephrine for Bronchiolitis, Cochrane Library, 2003; Issue 1. 4 Table 1 Results of Web- Based Search Author Date Country Numa A 2001 Australia Patient Group 15 patients Less than 2yrs Intubated, ventilated Proven RSV No bronchodilation for 12 hrs Wainwright 194 Patient 2002 > 12 months Australia N steroids for 24 hrs No Bronchodilation for 4 hrs Singh V 88 patients 2002 2-12 months old India Randomly given salbutamol or adrenaline nebs Sanchez I 24 patients 1993 Mean age 4.6 months Canada First episode of RSV Study Type Outcomes Key Results Study Weaknesses Prospective Cohort Resp mechanics: -Flow vol curves Decrease respiratory resistance No change in oxygen sats Prospective Cohort Length of hosp stay No significant effect No placebo Small study Patients intubated so unable to grade respiratory effort post treatment. Used three different nebuliser systems Prospective Cohort Clinical improvement - Resp rate - Sats - RDAI - clinical Clinical score Pulmonary mechanics Adrenaline showed more Initial assessment by clinical improvement than different people salbutamol. Prospective Cohort Adrenaline nebs showed greater improvement in clinical score and pulmonary mechanics than salbutamol. 5