Anaphylaxis - EM Tutorials
advertisement
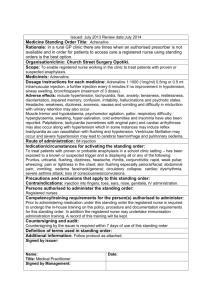
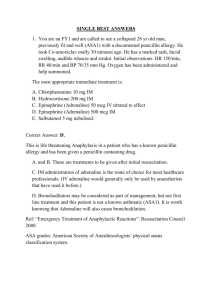
Anaphylaxis SHO presentation Tom Francis ICU Registrar Anaphylaxis • • • • • • What is it Pathophysiology Common causes / precipitants Features / signs Treatment After-care / discharge Anaphylactic shock • Type 1 IgE mediated (usually) hypersensitivity reaction • Chain Reaction • Release of histamine and other cytokines from mast cells and basophills • Causes contraction of bronchial smooth muscles, vasodilation of peripheral vasculature, capillary leak and cardiac muscle depression ADRENALINE • Mainstay of treatment is Adrenaline 0.5mg IM ADRENALINE Precipitants / causes • Drugs – Abx, cross reactivity B-lactams – Muscle relaxants – IV contrast • Food • Bee stings / wasp / horse fly IM injection UPPER OUTER THIGH DELTOID Recognition • Airway – Airway oedema – larynx, lips, tongue, eyelids – Stridor is a sign of airway obstruction • Breathing – Bronchial smooth muscle constriction – wheeze, respiratory distress, increased work of breathing • Circulation – Relaxation of vascular smooth muscle – Vasodilation, hypotension and erythema – Increased capillary permeability leading to loss of fluid from circulation : hypotension, tissue swelling, urticaria and Angioedema Urticaria Angioedema ADRENALINE • • • • 0.5mg IM Half of 1/1000 vial (the small one) Found in emergency box on all wards Can repeat every 5 mins 0.5mg ADRENALINE IM Adrenaline • α1 – peripheral vasoconstriction via smooth muscle constriction – Increased SVR • Β1 – Increased Cadiac output through +ve chrnontropy and inotropy • Β2 – Bronchial smooth muscle relaxation • Also acts directly on mast cells preventing further histamine release Promethazine (Phenergan) • 25mg slow IV injection (can use IM) • Sedating anti-histamine (H1) • Prevents capillary leak and helps treat hypotension due to loss of intravascular fluid • If persistant hypotension despite treatment with adrenaline can use ranitidine (H2) as second line. 50mg Ranitidine IV slowly Hydrocortisone • • • • 200mg IV hydrocortisone Requires reconstituion with sterile water OF NO VALUE IN IMMEDIATE RESUSCITATION Is of value to prevent rebound anaphylaxis though onset of several hours, should be given to prevent further deterioration in severely affected patients IV Fluids • Vasodilation and increased vascular permeability • 3rd spacing of fluid into interstitial space • DISTRIBUTIVE SHOCK • 1 litre Crystalloid or colloid STAT once Adrenaline given IM • 1 – 3 litres commonly required • 50mg Ranitidine can help persitant low BP Treatment ADRENALINE 0.5mg IM • Airway (and supplemental Oxygen) – nebulised adrenaline 5mg (5 x 1/1000) – Consider intubation. • Breathing – bronchospasm usually responds to adrenaline, can give nebulised salbutamol 5mg if wheeze persists. Treat as acute asthma • Circulation – – – – Raise legs / head down on bed if hypotension Large bore IV access 1 litre IVI stat 50mg Ranitine IV if persistant Treatment • Mainstay of treatment is Adrenaline 0.5mg IM ADRENALINE Where now? • Pts who require treatment for anaphylaxis need to be discussed with ICU • Rebound Anaphylaxis is a concern • Tryptase levels to confirm diagnosis – <1 Hour, 8 hours, 24 hours Discharge post anaphylaxis • Oral antihistamine e.g loratadine 3/7 • Oral Steroid 3/7 – Reduces risk of further reaction • Refer for specific allergy diagnosis • Epi-pen prescription – 300mcg Adrenaline Further Mx… • ACC form • Refer to GP for Medic Alert bracelet • Fill out an Alert/Adverse Reactions/Allergies form • Complete CARM report if a medication allergy – (Centre for adverse reactions monitoring) – https://nzphvc-01.otago.ac.nz/carm/ – Or easily found on google! Don’t forget!!! 0.5mg IM ADRENALINE Paediatrics • Adrenaline 0.01ml/kg of 1:1000 IM – Minimum 0.1 ml – Maximum 0.5 ml (10kg) (50kg) • Dose will be between 100 – 500mcg IM Airway obstruction • Sit child upright • Neb adrenaline 1:1000 0.5ml/kg, max 6ml. Dilute to at least 4ml Cardiovascular compromise • • • • • Poor perfusion, tachycardia, hypotension IV access – Consider IO 20ml/kg NaCl Rpt as required – 4% albumin after 2nd bolus Adrenaline infusion Bronchospasm • Salbutamol neb 5mg PRN/continuous • Consider IV salbutamol • Intubation / ventilation Further Mx • Hydrocortisone 4mg/kg IV Q6H • H1 antihistamine (loratadine / cetirizine) – Itch – Angioedema • PO Ranitidine 1-2mg/kg (max 150mg) in sever reactions • If require more than 1x dose Adrenaline require 24 hour admission References: • • • • ALS handbook (UK) ACLS level 7 handbook (NZ) NZ resuscitation website Starship PICU guidelines