Heliox therapy in bronchiolitis - Sheffield Children`s NHS Foundation
advertisement

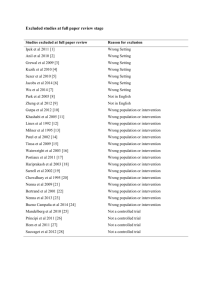
Journal Club 17/09/13 Rob Morton Heliox Therapy in Bronchiolitis: Phase III Multicentre double blind RCT Chowdhury et al. Pediatrics 2013; 131:661-669 Bronchiolitis season in Sheffield Photo removed for copyright reasons Bronchiolitis season in Sheffield Photos removed for copyright reasons Heliox • Airways in bronchiolitis oedematous and inflamed, lined/blocked with mucus. • Mix of 21% O2 and 79% Helium- Lighter than air or O2. • Promotes laminar rather than turbulent flow in congested airways. Also has a higher CO2/02 binary coefficient, may promote alveolar gas exchange. • Safe, inert • ? Cheap- $70 dollars a canister- 3-5 canisters a day • = £219 per day Heliox Cochrane review(2010) Liet et al. Heliox inhalation therapy for bronchiolitis in infants. Cochrane Database Syst Rev. 2010(4):DD006915 • 4 trials including children < 2 years • All on intensive care units • 3 studies showed improvements in symptoms scores at 1 hr of age • Concluded insufficient evidence, need for a large RCT BREATHE trial (The Bronchiolitis Randomized Controlled Trial Emergency-Assisted Therapy with Heliox— An Evaluation ) • 4 centres- UK & Australia • ? 3 Bronchiolitis seasons 2005-2008 Inclusion Criteria • All infants (<12months) with clinically diagnosed bronchiolitis by a doctor from A&E or wards • O2 sats <93% in air or • “Respiratory distress” • Requiring hospital admission Randomised to 2 groups Intervention “Controls” • “Heliox” via tight fitting face mask • Nasal cannulae if not tolerated • CPAP if requiring >4L/min O2 flow rate (mask), or >2L/min (NC) • “Airox”- same delivery criteria Outcomes Primary • “Length of time to alleviate hypoxia and respiratory distress”- time from start of trial gas to clinical stability out of O2 for 1 hour Secondary • Proportion of each treatment group requiring CPAP • Woods asthma score CASP (Critical Appraisal Skills Programme) • 1. Did the trial address a clearly focused issue? • Yes/No. • Does Heliox improve length of treatment in bronchiolitis? • Is that the relevant issue? Length of stay more important. • ? Severe/ mild bronchiolitics? • 2. Was the assignment of patients to treatments randomised? • ?Yes • Randomised but ?? not all accountable • ? Not all patients eligible approached for trial? • 4 centres, 3 seasons = 30 bronchiolitics per year. Adelaide has a population of 1.3million, Sheffield 0.5 million! • 3. Were all of the patients who entered the trial properly accounted for at the end of the trial? • ?Yes But… Is it worth continuing?? • ………?...........Yes • 4. Were patients, health workers and study personnel “blind” to the treatment? • Yes- Good blinding process. Canisters A & B. • ? Any smell to heliox? Presumably not. • 5. Were the groups similar at the start of the trial? Were the groups similar? • • • • Admitted from A&E? Previous bronchiolitis Time from start of symptoms? Co-morbidities? How are they fed? Bottle/ NG/ IV? Time since admission? • 6. Apart from the experimental intervention, were the groups treated equally? • ?- No mention of feeds, other cares. As study well blinded we can presume they were equal across the 2 groups. • How much O2 was required in each group, how severe were the patients? % O2 has an effect on use of Heliox. What are the results? • 7. How large was the treatment effect? What are the results? Outcomes • Length of treatment- Decreased in group who tolerated facemask, particularly those who are RSV+ve. • If tolerates facemask, and RSV+ve, LOT 1.46 vs 2.01 days, reduces length of treatment by 0.5 days • ? Decreases need for CPAP (not statistically significant and small numbers) • “ Reduced respiratory distress”, significant from 8 hrs. ?? Take their word for it. • 8. How precise was the treatment effect? • No Confidence intervals, IQR instead, as using medians. What are the results? 9. Can the results be applied to our local population? • Developed country, same patients and pathology • Standard care does not usually involve facemasks or CPAP on wards. • No comparison to standard care. • ? Can be used for bronchiolitics who are RSV +ve, if they can tolerate a face mask. May prevent need for CPAP & HDU admission? 10. Were all the clinically important outcomes considered? • No. • Length of treatment of limited use as no comparison to normal care. Need to know length of stay in hospital (impossible to do in this study as no admission/ discharge times) • Eg., does the intervention/ mask lead to a decrease in feeds and prolong admission? • How much heliox was used? 11. Are the benefits worth the harms and costs? • How much Heliox was actually used? 5 canisters seems a lot per day/ per patient. = $350 per day/ £223 Best intervention group = £312 (1.4 days) • How much extra cost for the nursing care to fit face mask? • How much cost for the additional HDU beds? So….How should a bronchiolitis trial be done? SABRE: Hypertonic Saline in Acute Bronchiolitis: A Randomised Controlled Trial and Economic Evaluation BREATHE • O2 <93% or resp distress • No time limit to recruit • No time of discharge • No economic evaluation SABRE • O2 <92% on admission • Strict 90 minute limit to recruit • Criteria for “SABRE” fit for discharge- includes feeds • Full economic evaluation Questions?