Assignments:
advertisement
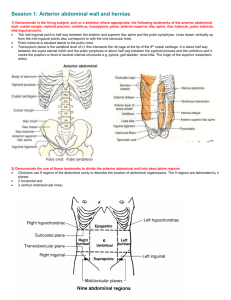
Assignments: 1. Complete the learning module entitled abdominal wall & inguinal region. Objectives: 1. Recognize and define the abdominal cavity, peritoneal cavity. Describe the divisions of the anterolateral abdominal wall. 2. Describe the general layers of the anterolateral abdominal wall and the relationships of the layers, partitions and compartments one encounters when dissecting from superficial to deep in any particular region. 3. Describe the blood supply and innervations of the anterolateral abdominal wall. 4. Recognize the anatomical structures related to incisions on anterolateral abdominal wall. 5. Recognize and define the inguinal region. Describe the general layers of the inguinal region and ligaments in this region. 6. Recognize and define the inguinal canal and the 4 walls and 2 openings of it. 7. Recognize and define the inguinal triangle. Procedure: 1. Study laboratory 35 and 36 (human anatomy). 2. Study plates 231-245 (interactive atlas). 3. Discuss the next questions in groups 1). Discuss the clinical cases on your textbook about anterolateral abdominal wall and inguinal region. 2). Discuss the cases below: Case 1 A 28-year-old woman in her 36th week of pregnancy arrived in the emergency room following an automobile accident. Immediately following the accident she went into labor. The accident had broken her pelvis such that the emergency room physician deemed a vaginal delivery would be hazardous. An obstetrician was called, and she agreed with the ER physician's initial assessment. A Cesarian section was performed, resulting in the delivery of a healthy baby girl. During the operation, the obstetrician used a Pfannenstiel incision to open the abdomen. This incision involves making a transverse, slightly convex cut large enough to deliver a child at approximately the pubic hairline. Questions to consider: 1. 2. 3. 4. What abdominal wall layers must be incised at the pubic hairline (near the midline) in order to access the abdominal cavity? Why is the incision made in a convex manner instead of straight across? What vascular structures might be cut during a Pfannenstiel incision? Where in the abdomen could a surgeon make a large vertical incision with minimal detrimental effect? Case 2 A twenty-five year-old female medical student presents to the emergency room with a complaint of "colicky" periumbilical pain which has intensified over the last 6-8 hours and now has started to migrate to the right lower quadrant. The patient reports some initial nausea, and as the pain has increased she has had increasing emesis and anorexia. Physical exam demonstrates the patient has no distension, auscultation reveals hyperactive bowel sounds, and on palpation the patient demonstrates abdominal guarding and rebound tenderness, and the muscles of the anterior wall in the right lower quadrant are rigid. In addition, the patient has a low-grade fever, and laboratory tests reveal a rising white blood cell count. The attending determines that the patient has acute appendicitis and prepares to take the student to the O.R. for an appendectomy. The surgeon asks you the following questions regarding the surgery. 1. 2. 3. 4. 5. 6. What is McBurney's point? What types of incisions can be made in the abdominal wall? Which of these incisions would be the most ideal for an appendectomy? When placing an incision in the abdominal wall, what nerves have to be identified? What would be a consequence of damage to the nerves? Suppose that the surgeon, in the process of the appendectomy, is unable to locate the appendix through the small incision he made in the right lower quadrant, so he decides to extend his incision several inches superiorly toward the rib cage. What is likely to result from such a procedure? What nerve is at risk when an incision is made at McBurney's point? What would be the long-term effects of damage to this nerve? Case 3 S.T., a 35-year-old man, was carrying furniture out to a moving van in preparation for his family's move to a new home. When S.T. strained to pick up a particularly heavy coffee table, he suddenly felt a sharp pain in his right groin. Later, he noticed that a painful bulge had developed in his groin which disappeared when he laid on his back. He did not like going to the doctor, so he ignored the condition. After several months, the pain and the bulge in his groin increased and he finally consented to see a physician. On examination, the physician observed a swelling which began about midway between the anterior superior iliac spine and the midline, progressed medially for about 4 cm, and then turned toward the scrotum . Taking the history and physical findings into account, the physician made a diagnosis of indirect inguinal hernia and scheduled S.T. for surgery. The hernia was successfully repaired, and S.T. was released from the hospital a few days later. 1. 2. 3. 4. 5. 6. What abdominal wall layers must be incised at the pubic hairline (near the midline) in order to access the abdominal cavity? What defines this hernia as an indirect inguinal hernia rather than a direct inguinal hernia? List the key features of each. What caused the bulge? What body layers would surround it as it proceeded into the scrotum and what abdominal layers are they derived from? Why would it be necessary to repair a hernia like the one described above as quickly as possible? How is the inguinal canal formed, and which structures are associated with the inguinal canal in the male? in the female? What is the definition of an inguinal hernia? What is the male to female ratio of incidence of direct inguinal hernias? 7. 8. 9. What are common causes of direct inguinal hernias? What are the boundaries of Hesselbach's (inguinal) triangle ? Do you know your eponyms? What are the following structures? (NOTE: FYI only - we will not exam on these) Poupart's ligament Cooper's ligament Gimbernat's ligament Colles' ligament Henle's ligament Hesselbach's ligament