Session 1 - Mosaiced.org
advertisement

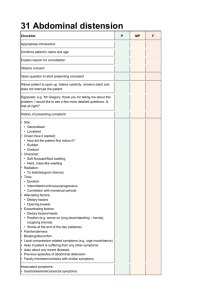
Session 1: Anterior abdominal wall and hernias 1) Demonstrate in the living subject, and on a skeleton where appropriate, the following landmarks of the anterior abdominal wall: costal margin, xiphoid process, umbilicus, transpyloric plane, anterior superior iliac spine, iliac tubercle, pubic tubercle, mid-inguinal point. The mid-inguinal point is half way between the anterior and superior iliac spine and the pubic symphysis. Lines drawn vertically up from the mid-inguinal points also correspond to with the mid-clavicular lines. Pubic tubercle is situated lateral to the pubic crest. Transpyloric plane is the vertebral level of L1 this intersects the rib cage at the tip of the 9 th costal cartilage. It is about half way between the supra sternal notch and the pubic synphysis or about half way between the xyphoid process and the umbilicus and it marks the position or level of several internal structures e.g. pyloris, gall bladder, renal hilia. The origin of the superior mesenteric artery. 2) Demonstrate the use of these landmarks to divide the anterior abdominal wall into descriptive regions Clinicians use 9 regions of the abdominal cavity to describe the location of abdominal organs/pains. The 9 regions are delineated by 4 planes: 2 horizontal and 2 vertical (midclavicular lines) The horizontal planes are: Subcostal plane passing through the inferior border of the 10th costal cartilage on each side. Transtubercular plane passing through the iliac tubercules and the body of L5 vertebra. These tubercles-approximately 5cm posterior to the anterior superior iliac spines (ASIS) – are usually palpable. The vertical planes are: Midclavicular plane passing from the midpoint of the clavicles to the midinguinal points – midpoints of the lines joining the anterior superior iliac spines and the superior edge of the pubic symphysis. Median line passing longitudinally through the body, dividing it into right and left halves. 3) Draw sketches to outline the arrangement of the external and internal oblique and transverse muscle layers, the rectus abdominis and rectus sheath, the transversalis fasciaa and the parietal peritoneum Picture not available on the internet. P179 in my anatomy book. Layers are skin, Campers fascia, Scarpas facia, deep fascia, external oblique, deep fascia, internal oblique, deep fascia, transverse, abdominal muscle, transversalis fascia, endoabdominal fat, parietal peritoneum. 4) Describe the rectus sheath and its contents The rectus abdominis muscle is enclosed in a sheath (known as the rectus sheath), which is formed by the aponeuroses of the 3 anterolateral muscles of the anterior abdominal wall. The aponeurosis of the transversus abdominis muscle pass behind the rectus muscle. The aponeurosis of the external oblique muscle passes in front of the rectus muscle. The aponeurosis of the internal oblique muscle is said to split such that half of its fibres pass behind and half pass infront of the rectus muscle. 5) Define the linea alba and the linea semilunaris The linea alba is a midline fibrous band at which the all 3 aponeurotic fibres fuse. The linea semilunaris is where they fuse at the lateral border of the rectus sheath 6) Explain the importance of the distinction between the fatty and membranous layers of the superficial fascia 7) Define the sources and distribution of the motor and sensory nerves to the abdominal wall and diaphragm The nerve supply to the anterior abdominal wall comes from the lower six intercostals nerves and the first lumbar nerves (T7-L1). These nerves run between the internal oblique and the transversus abdominis in the same way that the intercostals nerves run between the internal and innermost intercostals muscles. Some of the lowermost nerves cannot gain entry into this neurovascular layer immediately, because they first appear on the anterior surface of large posterior abdominal wall muscles that get in the way. The intercostals and subcostal nerves pass round the abdominal wall, cross the semilunaris and enter the restuc sheath and finally become cutanous here. Nerves in the anterior abdominal wall extend along the course of the ribs and costal cartilages. The uppse nerves run down towards the umbilicus (T10) or pubic symphysis (T12). L1 is the lowest nerve to supply muscles of the anterior abdominal wall but it just fails to reach the midline. 8) Explain the roles of the abdominal wall muscles including breathing and control of intra-abdominal pressure 9) Demonstrate in the living subject and in dissected material the nature and course of the inguinal canal making correct use of the following terms: superficial and deep inguinal rings, mid-inguinal point, pubic tubercle, testis, testicular vessels, scrotum, spermatic cord, ducuts deferens, round ligament of the uterus The inguinal canal in adults is an oblique, inferomedially directed passage through the inferior part of the anterolateral abdominal wall. It lies parallel and just superior to the medial half of the inguinal ligament. Inguinal ligament runs between the anterior superior iliac spine and the pubic tubercle. The main occupant of the inguinal canal is the spermatic cord in males and the round ligament of the uterus in females. The deep inguinal ring is the site of an outpouching of the transversalis fasciaapproximately 1.25cm superior to the middle of the inguinal ligament and lateral to the inferior epigastric artery. The superficial inguinal ring is a slit like opening between the diagonal fibres of the aponeurosis of the external oblique. Diagram on P195. The inguinal canal has a roof, floor and a posterior and anterior floor. Roof = internal oblique and transverse abdominal fibres. Floor = inguinal ligament Anterior wall = external oblique Posterior wall = transversalis fascia 10) Distinguish between direct and indirect inguinal hernias Hernia = the protrusion of a viscus through a decect from its containing compartment into an abnormal postion. Direct = weakness and thinning of the conjoint tendon (which forms the posterior wall of the canal medially), the hernia can bulge through the conjoint tendon and then directly through the superficial ring and into the scrotum. Indirect = occurs when the peritoneum lining the abdominal cavity enters the deep ring and protrudes through the inguinal canal , out through the superficial ring and into the scrotum. Identifying the tubercle and the position of the inferior epigastric artery allows the origin of each type of hernia to be diagnosed. At operation an indirect hernia passes lateral to the vessel and a direct hernia medial to the inferior epigastric artery. 11) Distinguish between acquired and congenital inguinal hernia Congenital - The descent of the testes requires the processus vaginalis, which is a fingerlike projection of parietal peritoneum. This fetal structure normally closes, however a persistently patent processus vaginalis is a ready-made indirect inguinal hernial sac. Acquired - Any cause of increased intra-abdominal pressure can exploit a weak abdominal wall, whether the weakness is purely due the presence of the inguinal canal or due to weakening of tissues with age, fatty infiltration associated with obesity or the increase in circulating elastases that have been postulated as a cause for weak abdominal musculature. The inguinal re is an area of weakness in the inferior part of the anterolateral abdominal wall, especially in males because of the passage of the spermatic cord through the inguinal canal. 12) Summarise the anatomical basis for femeral hernia Femoral hernia is more common in women than in men because the femoral ring is larger in women than in men because of the greater breadth of the female pelvis. The femoral ring is the usual originating site of a femoral hernia, a protrusion of abdominal viscera through the femoral ring into the femoral canal. A femoral henia appears as a mass, often tender, in the femoral triangle. The hernia is bounded by the femoral vein aterally and the reflected part of the inguinal ligament – the lacunar ligament – medially. Initally the hernia is small because it is contained within the femoral canal, but it can enlarge by passing inferiorly through the saphenous opening into the pubic tubercle, whereas an indirect inguinal hernia is superior to the inguinal ligament and may enter the scrotum. Strangulation of a femoral hernia may occur because of the sharp, rigid boundaries of the femoral ring, particularly the concave margin of the lacunar ligament. Strangulation of a femoral hernia interferes with the blood supply to the herniated intestine, and this vascular impairment may result in death of the tissues. 13) Describe the lymphatic drainage of the anterior abdominal wall Superficial lymphatic vessels accompany the subcutaneous veins, those superior to the umbilicus drain mainly to the axillary lymph nodes however, a few drain to the parasternal lymph nodes. Superficial lymphatic vessels inferior to the umbilicus drain to the superficial inguinal lymph nodes. Deep lymphatic vessels accompany the deep veins and drain to the external iliac, common iliac and lumbar lymph nodes.