Back pain flashcards
advertisement

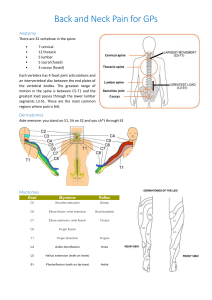
Back pain flashcards Jake Timothy Consultant Spine surgeon and Neurosurgeon Ganesh Baranihandaran Consultant Pain Specialist 1 Sciatica • -pain originating in the back and radiating down posterior or lateral thigh (sciatic nerve distribution) -many causes such as piriformis synd, lumbar spine probs 2 Radiculopathy • impairment of the nerve root leading to neurologic problems -paresthesia, numbness, change in Deep Tendon Reflexes 3 Spondylosis • Generic term for ‘wear and tear in the spine’ • Used too much for normal physiological ageing of the spine 4 Spondylolithesis • Lithesis meaning ‘to slip’ • When anterior displacement of one vertebra to another • Can be diagnosed by x-ray • If surgery is contemplated may need fusion procedure as well as decompression 5 Strain or sprain • Sprain affects the ligaments • Strain affects the muscles 6 Anatomy of disc • -nucleus pulposus = gel center -annulus fibrosus = surr + holds nuc pulp in -degen disc dz = less water, inc compression of discs with age -nerve roots leaving = one below until C8 and then becomes one above ex = C5/C6 = C6 nerve root ex = L5/S1 = L5 nerve root ex = T1/T2 = T1 nerve root 7 History of low back pain • -Onset -Location -Duration -Character -Ameliorating/Aggravating/Associated factors -Radiation -Timeline -Severity *OLD CARTS* -ROS = to rule things out 8 Differential diagnosis • *things to rule out first = -cauda equina synd, fracture, OM, infection, Cancer *Others = -herniated disc, scoliosis, SD, ankylosing spondylitis, visceral dz 9 Red flags • 1) Age > 50 = Fx, Cancer 2) Fever, recent infection = Infection 3) Significant trauma= Fx 4) Unrelenting night pain = Cancer, Fx 5) Progressive motor or sensory deficit = Cauda Equina, Cancer 6) Saddle Anesthesia= Cauda Equina 7) Difficulty urinating or fecal incontinence = Cauda Equina 8) Unexplained weight loss =Cancer 9) Hx or strong suspicion of cancer = Cancer 10) Hx of osteoporosis = Fx 11) Chronic oral steroids = Fx, Infection 12) IV drug use = Infection 10 Physical examination • -Gait and posture -Palpation -ROM -Sensation = Light touch and Pin prick -Strength -Deep tendon reflexes -Babinski (tells UMN deficit) -Heel walking and toe walking = asses neuro and strength *Special Tests -Straight Leg Test - seated and lying -FABER test -Trendelenburg 11 Neuro exam • • L1 Groin, iliopsoas, hip flexion L2 anterior thigh, iliopsoas, sartorius, hip adductors-hip flexion and adduction • L3 -Medial aspect of knee-Iliopsoas, quadriceps, sartorius, hip adductors-Hip flexion, knee extension, hip adduction • • • L4 = tibialis ant, patellar reflex, medial leg L5 = ext hallucis longus, front of foot S1 lateral leg, achilles reflex + eversion of foot 12 Lower motor neuron deficit • -Weakness - flaccid paralysis -DTR - decreased or absent -Babinski -absent -Atrophy - may be marked -Fasciculations - may be present **Typically spine probs affect LMNs 13 Upper motor neuron deficit • Weakness - Spastic paralysis DTR - Increased Babinski - Present Atrophy - absent or due to disuse Fasciculations - absent 14 Special tests • 1) Straight leg test - done seated, lying, or crossed (raise leg and see if use back to help) 2) FABER = flexion, abudct, ext rotation; testing hip + SI joint 3) Hoover's = try lift right, left will push down 15 Imaging options • *X ray = Boney architecture, fracture, osseous lesions *MRI = Soft tissue *CT= Fracture, prior lumbar surgery *Bone Scan = Cancer, osteomyelitis, stress fracture *Myelography = dye into epidural space to see compression; done only if CI to MRI 16 Cauda equina • *Reduction of volume of spinal canal -Compression of nerve roots -Muscle paralysis -Urinary or Bowel dysfunction *Causes = cancer, disc probs, hematoma *Symptoms -Radicular pain of both legs -Saddle anesthesia (butt and back of legs) -Difficulty voiding or loss of sphincter control -Leg weakness *Physical findings -Sensory changes -Difficulty standing -Difficulty with heel or toe walking *Tests -MRI**, X ray, CRP, CBC, ESR *Emergent surgical referral 17 Compression fracture • *High energy trauma *Type of compression fracture -Simple - anterior half of vertebral body -Burst - extending into the posterior third of the vertebral body -Posterior ligament disruption in flexion distraction injuries are unstable *Physical findings -Tenderness to palpation over the vertebra -Step off -Hematoma -Neuro exam 18 Acute low back pain • LBP < 6 weeks in duration *Causes -strain or sprain -twisting, repeated lifting, vibrating equipment (common = bending down and twisting) 19 Symptoms of low back pain • *Symptoms -LBP radiating into buttocks and posterior thighs -R/O red flags *Physical Exam -No neurologic deficit -Monitor flexion and extension -With or without sciatica 20 Tests and treatment for acute low back pain • *Tests -X ray not helpful *Treatment -Symptomatic Relief - including meds -Return to activity - NO bed rest 21 Only evidence based pharma treatments • NSAID’s • Paracetamol • Avoid codeine based tables as cause constipation and headaches • *Activity -Lifting, Stretches, Physical Therapy *Ice for 1st 24 hrs, then heat 20 min at a time *Spinal manipulation (OMT, Chiropractic) 22 Degenerative disc/ chronic • *LBP > 3 months duration *Recurrent and episodic symptoms *Symptoms -LBP radiating into the buttocks -Aggravated by activities -May have intermittent sciatica *Physical Exam -Lumbar or SI tenderness -Muscle spasm -Normal strength and neuro testing -Negative straight leg test -Deconditioning (no exercise makes it worse) 23 Cause of disc herniation • Lifting with twisting Over time Most commonly L4-5 (affects L5), L5-S1 (affects S1) - b/c affects exiting nerve root below not one that comes out at that point 24 Symptoms of acute disc • *Symptoms -Abrupt onset -Pain worse in leg than back -Radiating in dermatomal pattern = sciatica typ present (but if have sciatica, not necessarily have disc herniation) -Pain worse with valsalva -Worse with flexion!! *Physical Exam -May list when standing -Straight leg test - positive if lean back -Neurologic deficit - weakness, reflexes, sensory 25 Imaging of acute disc • -If red flags present→ immediately -After 4-6 week trial of conservative care -MRI, Myelography, CT 26 Treatment of acute disc • • *Activity -No bed rest *Medications -NSAIDs -Muscle relaxants -Gabapentin -Opioids *Physical Therapy -Therapeutic ultrasound -Transcutaneous electrical nerve stimulation (TENS) -Traction -Exercises *Spinal manipulation = but NO HVLA *Epidural spinal injections *Surgery to relieve nerve root compression 27 Spinal stenosis • Narrowing of the central spinal canal by bone or soft tissue with compression of nerve root 30% of those over 60 Most common at L2-3, L3-4, L4-5 28 Signs and symptoms of LCS • *Symptoms -Neurogenic claudication -Pain relieved with flexing forward (worse with extension!!) -May have spondylolisthesis *Physical Exam -Pulses normal -Reflexes may be decreased -Proprioception impaired - positive romberg -May have sensory changes 29 Treatment of spinal stenosis • -NSAIDS -Gabapentin -Physical Activity -Epidural Steroid injections *Surgery -Based on symptoms and other comorbidities -Spinal fusion if also spondylolisthesis or scoliosis 30 • Scoliosis -Lateral curvature of the spine - named by convexity side *Cause in adults -Degenerative spondylosis -Degenerative spondylolisthesis *Symptoms -Pain at region of deformity -Radicular symptoms usually L4 or L5 nerve root -Neuro symptoms less likely -Getting shorter, "hump" *Physical Exam -Postural exam -Palpate the spine *Treatment -NSAIDS -Exercise program -surgery if young 31 Spondylolithesis • *Anterior slippage of one vertebral body over the next *Degenerative -Degenerative of facet joints -Intervertebral disc changes -Lamina and pars interarticularis are intact *Physical exam -Loss of lordosis -Step off of spinal processes -Decreased reflexes -Weakness in toe or heel walking 32 Imaging and treatment • *Imaging -AP and lateral x ray -Lateral will show slippage *Treatment -NSAIDS -Exercise -Weight loss -Abdominal binder does not help! -Surgery = fusion 33