Functions of the Circulatory System
advertisement

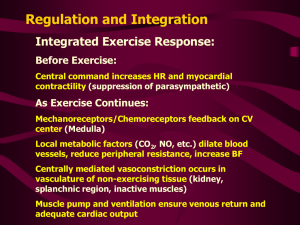
1 BLOOD FLOW AND THE CONTROL OF BLOOD PRESSURE Goal of cardiovascular regulation is the maintenance of adequate blood flow thru peripheral tissues and organs. Under normal circumstances blood flow is equal to cardiac output. o When cardiac output goes up blood flow goes up more blood thru capillaries more blood to tissue cells o When cardiac output declines blood flow goes down less blood thru capillaries less blood to tissue cells The afterload of the heart is determined by the interplay between pressure and resistance (forces like friction between blood and vessels that oppose blood flow) PRESSURE Blood is incompressible Hydrostatic pressure is generated by the force exerted in all directions against blood o If there was no resistance in the cardiovascular system, there would be no need for the heart to generate pressure to force the blood thru the systemic and pulmonary systems A pressure gradient does exist and blood flows from a high pressure to a low pressure The flow rate is directly proportional to the pressure gradient. o The greater the pressure, the faster the flow o The lower the pressure, the slower the flow In the systemic circuit (blood between heart and all tissues except lungs), the pressure gradient is the circulatory pressure (CP) o The pressure difference between the base of the ascending aorta and the entrance to the right atrium o Circulatory pressure averages around 100 mmHg o This pressure is needed primarily to force blood through the arterioles (resistance vessels) and into peripheral capillaries (where gas exchange takes place) Circulatory pressure is divided into 3 components: o Blood pressure (BP) This is arterial pressure (elastic & muscular arteries and arterioles) and ranges from an average of 100mm Hg to roughly 35 mm Hg at the start of the capillary network o Capillary pressure Pressure within the capillary beds. Along the length of a typical capillary (only place gas exchange is taking place), pressure declines from roughly 35 mm Hg to 18 mm Hg o Venous pressure Pressure within the venous system (venules & veins) Pressure gradient is low, from the venules to the right atrium it is only around 18 mm Hg As the blood flows away from the heart (left ventricle) the CP decreases and is almost 0 mm Hg when it returns back to the right atrium RESISTANCE A resistance is a force that opposes movement The resistance of the circulatory system opposes the movement of blood o the greater the resistance, the slower the blood flow For circulation to occur, the CP must be great enough to overcome the total peripheral resistance (the resistance of the entire CP) Because the resistance of the venous system is very low, we focus on the peripheral resistance (the resistance of the arterial system) For blood to flow into peripheral capillaries, blood pressure must be great enough to overcome PR The higher the PR, the lower the rate of blood flow Sources of PR include: o Vascular resistance The resistance of the blood vessels due to friction btwn blood and vessel walls Largest component of PR and depends on: Vessel length o Increasing length increases friction b/c the longer the vessel, the longer the surface area contact with blood o In adults, vessel length is constant Vessel diameter o Decreasing diameter (vasoconstriction) decreases blood flow b/c in small diameter vessels blood is slowed by friction in the narrow zone closest to the vessel wall 2 Increasing diameter (vasodilation) increases blood flow b/c blood near the center of the large diameter vessel will not encounter any resistance with the vessel wall Difference in diameter has much more significant effects on resistance than difference in length If there are two vessels of equal diameter (one 2 ‘x longer than the other), the longer vessel will offer 2x’s as much resistance to blood flow With 2 vessels of equal length, one 2x’s the diameter of the other, the smaller one will offer 16x’s as much resistance to blood flow See Fig. 15-14 Most PR occurs in the arterioles by altering the diameter of the vessels to control PR & blood flow Vasodilation decreases PR increases blood flow Vasoconstriction increases PR decreases blood flow o o Viscosity of blood (how thick it is) Resistance to blood flow due to the interactions among molecules and suspended materials in blood more water, less viscous decrease PR higher rate of blood flow less water, more viscous increase PR lower rate of blood flow Under normal circumstances, the viscosity of blood remains stable Dehydration less water more viscous decrease blood flow Anemia due to blood loss too few RBC’s less viscous increase blood flow Polycythemia too many RBC’s more viscous decrease blood flow Turbulence High flow rates, irregular surfaces (plaque build up in vessels), or sudden changes in vessel diameter upset the smooth flow of blood creates eddies and swirls = turbulence Normally turbulence occurs when blood flows between atria and ventricles and between the ventricles and the aortic and pulmonary trunks generating the third and fourth heart sounds o Third sound by vibrations of the ventricular walls o Fourth sound by the accelerated rush of blood into the ventricles o The first and second heart sounds are created by the opening and closing of the heart valves First sound due to AV valves closing and SV valves opening (at beginning of systole) “Lub” Second sound due AV valves opening and SV valves closing (at end of systole) “Dub” Turbulent flow across a damaged or misaligned heart valve is responsible for heart murmurs Rushing, gurgling, or whooshing sound due to malfunctioning heart valves o Incomplete closure of valve causing regurgitation of blood o Stenotic valve (too narrow) usually heard just BEFORE systole Turbulence develops in large arteries (aorta), when CO and arterial flow rates are high, seldom occurs in smaller vessels unless their walls are damaged o Scar tissue from a damaged vessel o Development of atherosclerotic plaque o Both create turbulence and restrict blood flow MEAN ARTERIAL PRESSURES or BP Arterial pressures overcome PR and maintain blood flow thru capillary beds Arterial pressure is not stable Rises during ventricular systole Falls during ventricular diastole See Fig. 15-5 Peak blood pressure measured during ventricular systole is called systolic pressure Minimum blood pressure at the end of ventricular diastole is called diastolic pressure When BP is recorded by listening for Korotkoff sounds in the brachial artery using a sphygmomanometer (BP cuff & press. gauge, along with a stethoscope), systolic and diastolic pressures are separated by a slashmark o See Fig. 15-7 o Systolic press. = 120 mm Hg o Diastolic press. = 80 m Hg Expressed as Syst/Diastol. 120/80 = average/normal BP 3 The difference between the systolic press. and diastolic press. is called the pulse pressure o PP = Systolic press – Diastolic press o PP = 120-80 = 40 To report a single valve for BP, the mean arterial pressure (MAP) is used o MAP is calculated by adding 1/3 of the pulse pressure to the diastolic press o MAP or MBP = diastolic + 1/3 (pulse pressure) MAP or MBP = diastlolic +1/3 (systolic – diastolic) MBP = 80 + 1/3 (120-80) or 80 + (40/3) MBP = 93.33 or 93 o The MBP is a function of cardiac output and total peripheral resistance o Remember TPR depends on the diameter of the blood vessels and viscosity of blood MBP = cardiac output x TPR MBP = (HR x SV) x TPR Elastic rebound o As systolic pressure climbs, the atrial walls stretch (like an extra puff of air expands a partially inflated balloon) o This expansion allows the arterial system to accommodate some of the blood provided by the ventricular system o When diastole begins & pressure falls, the arteries recoil to their original dimensions o Because the aortic semilunar valve prevents the return of blood to the heart, the arterial recoil pushes blood toward the capillaries o See Fig. 15-8 o MBP provides us with information on the heart’s pumping efficiency and the condition of the vessels in the systemic circuit Since systolic press indicates the contraction force of the heart and diastolic press indicates the condition of the blood vessels, and increase in the diastolic press indicates a decrease in vessel elasticity (i.e. hardening of the arteries) As a person ages the elastic arteries lose their elasticity; therefore, and as a persons gets older there may be an increase in blood pressure is largely due to the overall loss of vessel elasticity Partly due to increased deposits of cholesterol and other lipids in the blood vessel walls Hypertension is the presence of abnormally high blood pressure 130/85 Hypotension abnormally low blood pressure sometimes due to overaggressive treatment for hypertension CARDIOVASCULAR REGULATION Homeostatic mechanisms regulate cardiovascular activity to ensure that tissue blood flow meets the demand for oxygen and nutrients in the capillary beds (only place for gas exchange with tissues) The 3 variable factors that ensure these demands are cardiac output, peripheral resistance, & BP When cells become active, blood flow to that region must increase to deliver necessary O 2 and nutrients and to carry away CO2 and wastes generated by cellular respiration o When cells are not as active, blood flow to that region can be decreased o See Fig. 15-15 Goal of cardiovascular regulation is to ensure blood flow changes occur o At an appropriate time o In the right area o Without drastically altering blood pressure and blood flow to any vital organs (See Fig. 15-13) Factors involved in the regulation of cardiovascular function include o Local factors Change the pattern of blood flow within capillary beds in response to chemical changes in the interstitial fluids The is an example of autoregulation within the microcirculation at the tissue level (See Fig. 15-3 and 15-15) Arterioles metarterioles (thoroughfare channels) true capillaries venules Precapillary sphincters control blood flow at entrance to true capillaries via constriction or dilation Vasodilators Factors that promote dilation of precapillary sphincters called vasodilators 4 o When produced at the tissue level accelerate blood flow thru tissue of origin Examples: o Decr. tissue O2 levels o Incr. tissue CO2 levels o Generation of lactic acid or other acids by tissue cells o Release of nitric acid from endothelial cells o Rising concentrations of K+ or H+ in interstitial fluid o Chemicals released during local inflammation Histamine & nitric oxide o Elevated local temperatures Vasoconstrictors Aggregating platelets and damaged tissues produce compounds that stimulate constriction of precapillary sphincters (prevent blood loss and can be in response to pain) o Prostaglandins and thromboxanes o Serotonin (platelet aggregation) and Substance P (pain) Central mechanisms The nervous system is responsible for adjusting cardiac output and peripheral resistance to maintain adequate blood flow to vital tissues and organs Centers responsible for these regulatory activities include: Cardiac centers in medulla o Cardioacceleratory center increases cardiac output by increasing sympathetic innervation o Cardioinhibitory center decreases cardiac output by increasing parasympathetic innervation Vasomotor centers in medulla o Control of vasoconstriction Neurons innervating peripheral blood vessels release NE (adrenergic) Stimulation of receptor on smooth muscles in vessel walls of arterioles vasoconstriction. o Control of vasodilation Neurons innervating peripheral blood vessels release LESS NE (decreased sympth. stimul.) Less stimulation of receptors on smooth muscles in vessel wall of arterioles vasodilation Both work together and sometimes independently of one another See Fig. 15-22 and 15-23 Baroreceptor Reflex Baroreceptors are specialized receptors that monitor the degree of stretch in the walls of distensible organs The baroreceptors involved in cardiovascular regulation are located in the walls of the: o Carotid sinuses near the bases of the internal carotid arteries o Aortic sinuses in the walls of the ascending aorta o Wall of the right atrium o See Fig. 15-21 These receptors are components that adjust cardiac output and peripheral resistance to maintain normal arterial pressure See Fig. 15-22: Response to increased blood pressure When BP rises more stretch on barorecptors more stimulation send to CV o Decrease in sympathetic output & increase in parasympathetic output Vasodilation, decreased force of contraction in ventricular myocardium, decreased heart rate at SA node decreased PR and CO Results in decreased BP It is a negative feedback loop See Fig. 15-23: Response to decreased blood pressure (orthostatic hypotension) BP lowest with lying down due to equal forces of gravity all over body o Heart does not have to work as hard to pump blood back up against gravity BP highest when standing due to blood having to overcome forces of gravity to get blood back to heart via venous return BP increases when go from lying down, to sitting, to standing 5 o When you stand up, blood pools in lower extremities thus creating an instantaneous decrease in venous return causing a decrease in BP. This is called orthostatic hypotension When BP falls less stretch on baroreceptors less stimulation send to CV o Increase in sympathetic output and decrease in parasympathetic output Vasoconstriction, increased force of contraction in ventricular myocardium, increased heart rate at SA node increased PR and CO Results in increased BP back to normal What would happen with the baroreceptor reflex and BP, if elasticity is lost in the arteries or arterioles? [HINT: less elastic = less stretch] o Chemoreceptor reflexes Responds to changes in the CO2, O2, and pH levels in the blood and cerebrospinal fluid Chemoreceptors involved are sensory neurons located in the carotid bodies in carotid sinus and aortic bodies in aortic sinus When chemoreceptors detect increase levels of CO2 or decrease in pH CV centers stimulated results in an elevation in arterial pressure via stimulation of vasomotor center Strong chemoreceptor stimulation (decrease in O2 levels) more widespread sympathetic stimulation increasing H.R. and C.O. o Endocrine factors Provides both long and short term regulation of cardiovascular performance Epinephrine & Norepinephrine from the adrenal medulla stimulate cardiac output & peripheral resistance Other hormones regulating CV function: Antidiuretic hormone (ADH) released in response to decrease in BP or increase in osmotic concentration of plasma o Results in peripheral vasoconstriction increasing BP o Also stimulates kidney’s to reabsorb water preventing a decrease in blood volume further increases BP Angiotension II appears in blood following release of rennin in response to decrease in renal BP results in vasoconstriction and raises BP o Stimulates secretion of ADH and aldosterone (reabsorption of Na+ in kidneys) o Stimulates thirst additional water consumed w/ presence of ADH to retain water elevates plasma volume increasing BP