Physio Chap 14 [10-26
advertisement
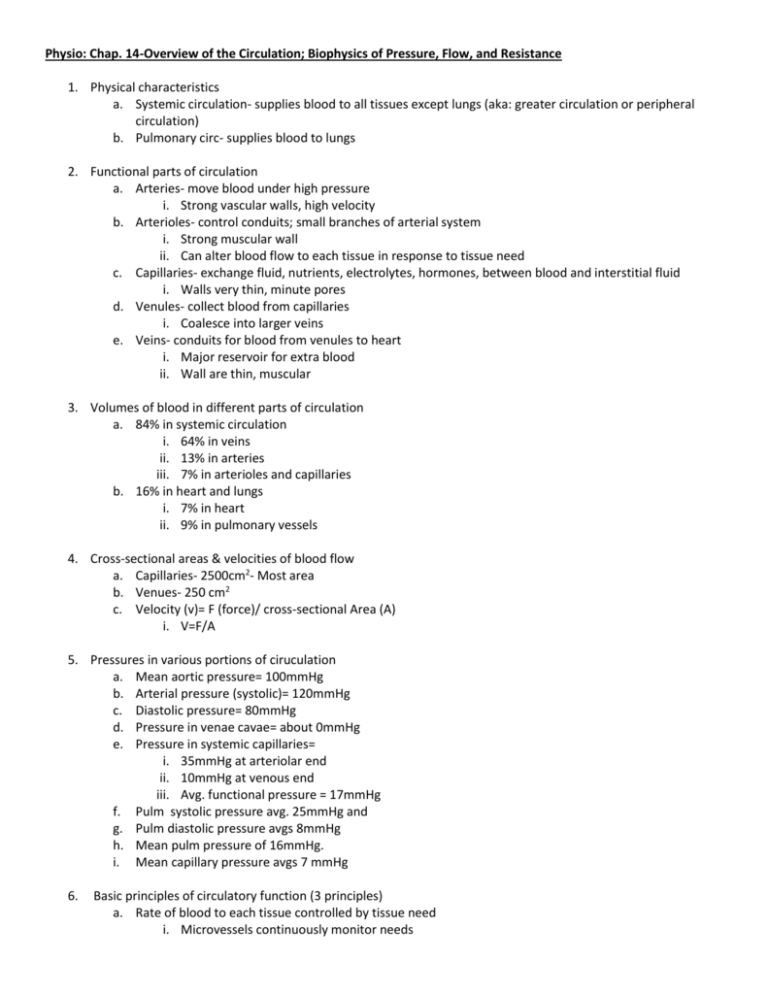
Physio: Chap. 14-Overview of the Circulation; Biophysics of Pressure, Flow, and Resistance 1. Physical characteristics a. Systemic circulation- supplies blood to all tissues except lungs (aka: greater circulation or peripheral circulation) b. Pulmonary circ- supplies blood to lungs 2. Functional parts of circulation a. Arteries- move blood under high pressure i. Strong vascular walls, high velocity b. Arterioles- control conduits; small branches of arterial system i. Strong muscular wall ii. Can alter blood flow to each tissue in response to tissue need c. Capillaries- exchange fluid, nutrients, electrolytes, hormones, between blood and interstitial fluid i. Walls very thin, minute pores d. Venules- collect blood from capillaries i. Coalesce into larger veins e. Veins- conduits for blood from venules to heart i. Major reservoir for extra blood ii. Wall are thin, muscular 3. Volumes of blood in different parts of circulation a. 84% in systemic circulation i. 64% in veins ii. 13% in arteries iii. 7% in arterioles and capillaries b. 16% in heart and lungs i. 7% in heart ii. 9% in pulmonary vessels 4. Cross-sectional areas & velocities of blood flow a. Capillaries- 2500cm2- Most area b. Venues- 250 cm2 c. Velocity (v)= F (force)/ cross-sectional Area (A) i. V=F/A 5. Pressures in various portions of ciruculation a. Mean aortic pressure= 100mmHg b. Arterial pressure (systolic)= 120mmHg c. Diastolic pressure= 80mmHg d. Pressure in venae cavae= about 0mmHg e. Pressure in systemic capillaries= i. 35mmHg at arteriolar end ii. 10mmHg at venous end iii. Avg. functional pressure = 17mmHg f. Pulm systolic pressure avg. 25mmHg and g. Pulm diastolic pressure avgs 8mmHg h. Mean pulm pressure of 16mmHg. i. Mean capillary pressure avgs 7 mmHg 6. Basic principles of circulatory function (3 principles) a. Rate of blood to each tissue controlled by tissue need i. Microvessels continuously monitor needs b. Cardiac output controlled by sum of all local tissue flows i. Heart responds to need ii. Uses nerve signals to pump required blood correctly c. Arterial pressure regulation independent of local or cardiac output control i. Nerves: 1. Increase force of heart pump 2. Cause contraction of large venous reservoirs (send blood to heart) 3. Generalized constriction of most arterioles a. More blood accumulates in arteries to increase arterial pressure ii. Kidneys essential in BP control 7. Interrelationships of pressure, flow, and resistance a. Flow through vessels determined by: i. Pressure gradient- pressure difference in blood between 2 ends of vessel ii. Vascular resistance- impediment to flow through vessel iii. F (flow) = P1-P2/R (resistance) 1. P1= origin of vessel pressure 2. P2= other end of vessel pressure 3. Flow decreases as resistance increases 4. The larger the pressure differences the greater the flow iv. Overall blood flow of adult= 5000ml/min= cardiac output v. Cardiac output- blood pumped into aorta each minute b. Electromagnetic flowmeter i. Vessel placed between poles of magnet ii. electrodes placed on either side of vessel perpendicular to magnetic lines of force c. Ultrasonic Doppler flowmeter i. Determines velocity by measuring frequency difference in transmitted wave and reflected wave ii. Doppler effect- reflected waves have lower frequency than transmitted waves because red blood cells move away from transmitted wave 8. Laminar flow of blood in vessels a. Blood flows in equal distances away from vessel wall (streamlined)- opposite to turbulent flow b. Central most portion of blood stays in center of vessel 9. Parabolic velocity profile during laminar flow a. Flow in center of vessel is greater than next to wall b. Flow very slow at edge next to wall due to adherence to wall 10. Turbulent flow under some conditions a. Rate of flow too great b. Sharp turns in vessels c. Passes over rough surface (atherosclerotic plaques) d. Forms whorls in blood (eddy current)= greater resistance= + friction e. Turbulent flow affected by velocity, diameter, density of blood, and viscosity of blood i. Re (reynold’s number) = v*d*p/ n 1. Re= tendency to turbulent flow, v=velocity, n= viscosity, d= diameter, p=density 2. High RE (200-400) = turbulence in aorta, & pulmonary artery 11. Blood pressure a. Force exerted by blood against are of vessel wall b. 1mmHg= 1.36cm of water pressure c. Measuring tools i. Mercury manometers not as accurate but cheap- good for recording steady pressures only ii. Electronic pressure transducer-more accurate 12. Resistance to blood flow a. A 13. Total peripheral vascular resistance and total pulmonary vascular resistance a. Pressure difference between systemic arteries and system veins= 100 mmHg b. Cardiac output of adult= 100ml/sec c. Total peripheral resistance= 100/100= 1 peripheral resistance unit (PRU) d. Mean pulm arterial pressure= 16 e. Mean left arterial pressure = 2 f. Net pressure difference 16-2= 14 g. 14/cardiac output (100)= 0.14PRU= total pulmonary vascular resistance 14. Conductance of blood flow a. Measure of blood flow through vessel for given pressure difference b. Conductance= reciprocal of resistance = 1/R c. Conductance increases to fourth power of diameter d. Poiseuille’s Law- blood touching vessel wall moves slower. Those in center move faster i. Increased diameter causes more to move faster in center ii. Rate of flow is proportional to fourth power of radius 1. diameter has greatest role in determining rate of flow e. Vessel diameter determines arteriolar resistance i. Arterioles are gate keepers 15. Vessel diameter and fourth power law in arteriolar resistance a. 2/3 total systemic resistance is arteriolar in small arterioles b. 4 fold increase in arteriolar diameter increases flow by 256-fold i. =very small increases in diameter make big difference in flow 16. Resistance to flow in series and parallel vascular circuits a. Arteriesarteriolescapillariesvenulesveins= arranged in series i. Flow in each is same and resistance to flow= sum of resistances of each vessel: 1. Rtotal = R1 + R2 + R3 + … b. Capillaries and blood supply to many tissues is arranges in parallel i. Allows each tissue to regulate its own blood flow 1. 1/Rtotal = 1/R1 + 1/R2 + 1/R3 + … 2. Total resistance is far less than resistance of each vessel 3. Increasing resistance of one vessel increases total resistance c. Conductance occurs because its easier for many vessels to flow in parallel than one large vessel to supply tissue its nutrients i. Multiple tissues and organs make up total conductance ii. If amputation occurs = reduced vascular conductance because you removed one part of the parallel circuit iii. Ctotal = C1 + C2 + C3 + … 17. Effect of blood Hematocrit and blood viscosity on vascular resistance and blood flow a. Increased viscosity = reduced blood flow b. Normal blood = viscosity 3x greater than water c. Viscosity of plasma= 1.5x greater than water d. Viscosity occurs because of many red cells in blood e. Hematocrit i. Portion of blood that is red cells ii. Men = 42 iii. Women = 38 f. Effects of Hematocrit on blood viscosity i. Viscosity increases as Hematocrit increases ii. Polycythemia= increased Hematocrit=increased viscosity= reduced flow g. Viscosity also affected by: i. Plasma protein concentration ii. Types of proteins in plasma 18. Effects of pressure on vascular resistance and tissue blood flow a. Rise in arterial pressure increases: i. force of contraction ii. vascular resistance b. Drop in arterial pressure decreases: i. Vascular resistance ii. Blood flow is maintained (blood flow autoregulation) c. Decreases in flow caused by: i. strong sympathetic stimulation (constricts vessels) ii. Hormonal vasoconstrictors 1. Norepinephrine- from adrenal medulla & CNS (as neurotransmitter) 2. angiotensin II- from rennin (in kidneys) and angiotensinogen=angiotensin I contverted to angiotensin II 3. Vasopressin- from hypothalamus and stored in posterior pituitary 4. Endothelin- from endothelium 19. Pressure- flow relationship in passive vascular bed a. Increased arterial pressure increases force and distends vessels (veins) decreasing vascular resistance b. Decreased arterial pressure increases resistance (elastic vessels collapse) i. Critical closing pressure- flow ceases as vessels completely collapse ii. Sympathetic stimulation & other vasoconstrictors can alter passive pressure-flow relationship iii. Inhibition of sympathetic activity dilates vessels and increases blood flow