Sherwood 10
advertisement

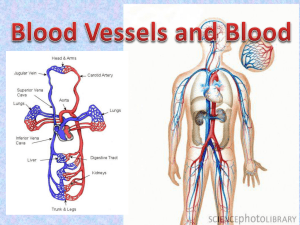
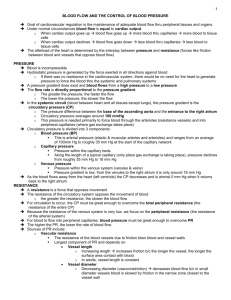
Chapter 10 The Blood Vessels and Blood Pressure Human Physiology by Lauralee Sherwood ©2007 Brooks/Cole-Thomson Learning Outline • • • • • • • Vessel types and flow Arteries Blood pressure Arterioles Capillaries Lymphatic system Veins Outline • Vessel types and flow – Vessel anatomy – Flow, flow rate, pressure gradients – Blood distribution, Poiselle’s law Human Coronary Artery. LM X6. Human artery showing atherosclerosis. LM X3. Human artery cross-section, elastic tissue stain. X80. Credit: © Biodisc/Visuals Unlimited 213940 Red and white blood cells within an arteriole. Arteries branch into arterioles within organs and deliver blood to the capillaries. SEM X6130. Artery and Vein. A distributing artery (right) and a medium-sized vein (left) surrounded by connective tissue. Arteries and veins are part of the extensive network of vessels that make up the vascular system. SEM X305. Credit: © Dr. Richard Kessel & Dr. Randy Kardon/Tissues & Organs/Visuals Unlimited 900019 Blood Flow • Blood is constantly reconditioned so composition remains relatively constant • Reconditioning organs receive more blood than needed for metabolic needs – Digestive organs, kidneys, skin – Adjust extra blood to achieve homeostasis • Blood flow to other organs can be adjusted according to metabolic needs • Brain can least tolerate disrupted supply Distribution of Cardiac Output at Rest Blood Flow • Flow rate through a vessel (volume of blood passing through per unit of time) is directly proportional to the pressure gradient and inversely proportional to vascular resistance F = ΔP R F = flow rate of blood through a vessel ΔP = pressure gradient R = resistance of blood vessels Blood Flow • Pressure gradient is pressure difference between beginning and end of a vessel – Blood flows from area of higher pressure to area of lower pressure • Resistance is measure of opposition of blood flow through a vessel – Depends on three things • Blood viscosity, vessel length, vessel radium – Major determinant of resistance to flow is vessel’s radius – Slight change in radius produces significant change in blood flow R is proportional to 1 r4 Relationship of Resistance and Flow to Vessel Radius Vascular Tree • Closed system of vessels • Consists of – Arteries • Carry blood away from heart to tissues – Arterioles • Smaller branches of arteries – Capillaries • Smaller branches of arterioles • Smallest of vessels across which all exchanges are made with surrounding cells – Venules • Formed when capillaries rejoin • Return blood to heart – Veins • Formed when venules merge • Return blood to heart Basic Organization of the Cardiovascular System Outline • Arteries – “pressure reservoir” – anatomy Arteries • Specialized to – Serve as rapid-transit passageways for blood from heart to organs • Due to large radius, arteries offer little resistance to blood flow – Act as pressure reservoir to provide driving force for blood when heart is relaxing • Arterial connective tissue contains – Collagen fibers » Provide tensile strength – Elastin fibers » Provide elasticity to arterial walls Arteries as a Pressure Reservoir Outline • Blood pressure – Systolic/diastolic – Measurements • Pressure and pulse – Mean arterial pressure – Pressure abnormalities Blood Pressure • Force exerted by blood against a vessel wall – Depends on • Volume of blood contained within vessel • Compliance of vessel walls • Systolic pressure – Peak pressure exerted by ejected blood against vessel walls during cardiac systole – Averages 120 mm Hg • Diastolic pressure – Minimum pressure in arteries when blood is draining off into vessels downstream – Averages 80 mm Hg Blood Pressure • Can be measured indirectly using sphygmomanometer • Korotkoff sounds – Sounds heard when determining blood pressure – Sounds are distinct from heart sounds associated with valve closure Blood Pressure Pulse Pressure • Pressure difference between systolic and diastolic pressure • Example – If blood pressure is 120/80, pulse pressure is 40 mm Hg (120mm Hg – 80mm Hg) • Pulse that can be felt in artery lying close to surface of skin is due to pulse pressure Mean Arterial Pressure • Average pressure driving blood forward into tissues throughout cardiac cycle • Formula for approximating mean arterial pressure Mean arterial pressure = diastolic pressure + ⅓ pulse pressure At 120/80, mean arterial pressure = 80 mm Hg + ⅓ (40 mm Hg) = 93 mm Hg Outline • Arterioles – Resistance vessels – Vasoconstriction and vasodilation – Regulation of arteiolar diameter • Local factors • Endothelial cells, nitric oxide Arterioles • Major resistance vessels • Radius supplying individual organs can be adjusted independently to – Distribute cardiac output among systemic organs, depending on body’s momentary needs – Help regulate arterial blood pressure Arterioles • Mechanisms involved in adjusting arteriolar resistance – Vasoconstriction • Refers to narrowing of a vessel – Vasodilation • Refers to enlargement in circumference and radius of vessel • Results from relaxation of smooth muscle layer • Leads to decreased resistance and increased flow through that vessel Arteriolar Vasoconstriction and Vasodilation Arterioles • Only blood supply to brain remains constant • Changes within other organs alter radius of vessels and adjust blood flow to organ • Local chemical influences on arteriolar radius – Local metabolic changes – Histamine release • Local physical influences on arteriolar radius – Local application of heat or cold – Chemical response to shear stress – Myogenic response to stretch Magnitude and Distribution Of the Cardiac Output at Rest and During Moderate Exercise Arterioles • Specific local chemical factors that produce relaxation of arteriolar smooth muscle – Decreased O2 – Increased CO2 – Increased acid – Increased K+ – Increased osmolarity – Adenosine release – Prostaglandin release Arterioles • Local vasoactive mediators – Endothelial cells • Release chemical mediators that play key role in locally regulating arteriolar caliber • Release locally acting chemical messengers in response to chemical changes in their environment • Among best studied local vasoactive mediators is nitric oxide (NO) Functions of Endothelial Cells Functions of Nitric Oxide (NO) Arterioles • Extrinsic control – Accomplished primarily by sympathetic nerve influence – Accomplished to lesser extent by hormonal influence over arteriolar smooth muscle Arterioles • Cardiovascular control center – In medulla of brain stem – Integrating center for blood pressure regulation • Other brain regions also influence blood distribution – Hypothalamus • Controls blood flow to skin to adjust heat loss to environment • Hormones that influence arteriolar radius – Adrenal medullary hormones • Epinephrine and norepinephrine – Generally reinforce sympathetic nervous system in most organs • Vasopressin and angiotensin II – Important in controlling fluid balance Outline • Capillaries – Exchange and anatomy – Pressures driving diffusion Capillaries • Thin-walled, small-radius, extensively branched • Sites of exchange between blood and surrounding tissue cells – Maximized surface area and minimized diffusion distance – Velocity of blood flow through capillaries is relatively slow • Provides adequate exchange time – Two types of passive exchanges • Diffusion • Bulk flow • Factors affecting diffusion – Ficks law of diffusion – Slow blood velocity – Permeability – Metarterioles and precapillary sphincters – Exchanges • Blood to interstitial fluid to cell – Passive – Active – Bulk Flow • Ultrafiltration • reabsorption Table 3-1, p. 62 Fig. 10-16, p. 355 Capillary blood pressure Plasma colloid osmotic pressure Interstitial fluid hydrostatic pressure Interstitial fluid colloid osmotic pressure Fig. 10-22, p. 359 Fig. 10-9, p. 345 Arteriole Smooth muscles Precapillary sphincter Metarteriole Myogenic tone Stopcock Local metabolic changes Capillary Venule Fig. 10-19, p. 357 Capillaries • Narrow, water-filled gaps (pores) lie at junctions between cells • Permit passage of water-soluble substances • Lipid soluble substances readily pass through endothelial cells by dissolving in lipid bilayer barrier • Size of pores varies from organ to organ Capillaries • Under resting conditions many capillaries are not open • Capillaries surrounded by precapillary sphincters • Contraction of sphincters reduces blood flowing into capillaries in an organ • Relaxation of sphincters has opposite effect • Metarteriole – Runs between an arteriole and a venule Outline • Lymphatic system – Drainage of tissue – Immune function – Edema Lymphatic System Lymphatic System • Extensive network of one-way vessels • Provides accessory route by which fluid can be returned from interstitial to the blood • Initial lymphatics – Small, blind-ended terminal lymph vessels – Permeate almost every tissue of the body • Lymph – Interstitial fluid that enters a lymphatic vessel • Lymph vessels – Formed from convergence of initial lymphatics – Eventually empty into venous system near where blood enters right atrium – One way valves spaced at intervals direct flow of lymph toward venous outlet in chest Lymphatic System • Functions – Return of excess filtered fluid – Defense against disease • Lymph nodes have phagocytes which destroy bacteria filtered from interstitial fluid – Transport of absorbed fat – Return of filtered protein To venous system Interstitial fluid Arteriole Tissue cells Venule Blood capillary Initial lymphatic Fig. 10-24, p. 362 Fluid pressure on the outside of the vessel pushes the endothelial cell’s free edge inward, permitting entrance of interstitial fluid (now lymph). Overlapping endothelial cell Interstitial fluid Lymph Fluid pressure on the inside of the vessel forces the overlapping edges together so that lymph cannot escape. Fig. 10-24, p. 362 Edema • Swelling of tissues • Occurs when too much interstitial fluid accumulates • Causes of edema – Reduced concentration of plasma proteins – Increased permeability of capillary wall – Increased venous pressure – Blockage of lymph vessels Outline • Veins – Capacitance vessels – Regulation of pressure and flow – Venous return Veins • Venous system transports blood back to heart • Capillaries drain into venules • Venules converge to form small veins that exit organs • Smaller veins merge to form larger vessels • Veins – Large radius offers little resistance to blood flow – Also serve as blood reservoir Pulmonary vessels 9% Systemic arteries 13% Systemic arterioles 2% Heart 7% Systemic capillaries 5% Systemic veins 64% Capacitance! Fig. 10-27, p. 364 Veins • Factors which enhance venous return – Driving pressure from cardiac contraction – Sympathetically induced venous vasoconstriction – Skeletal muscle activity – Effect of venous valves – Respiratory activity – Effect of cardiac suction Skeletal muscle pump Fig. 10-29, p. 366 Effects of Gravity Fig. 10-30, p. 367 Standing Walking Heart Thigh 150 cm Calf 34 cm Foot 100 mm Hg Foot vein supporting column of blood 1.5 m (150 cm) in height Venous pressure in foot 27 mm Hg Foot vein supporting column of blood 34 cm in height Fig. 10-31, p. 367 Vein Open venous valve permits flow of blood toward heart Contracted skeletal muscle Closed venous valve prevents backflow of blood Stepped art Fig. 10-32, p. 368 Respiratory activity and venous return 5 mm Hg less than atmospheric pressure Atmospheric pressure 5 mm Hg less than atmospheric pressure Atmospheric pressure Cardiac suction also Fig. 10-33, p. 368 Factors that Influence Venous Return summary Blood pressure Mean Arterial Pressure • Blood pressure that is monitored and regulated in the body – Regulation is important: • Provides adequate driving pressure (brain and organs) • Prevents extra work • Primary determinants – Cardiac output – Total peripheral resistance Mean arterial pressure = cardiac output x total peripheral resistance Determinants of Mean Arterial Pressure Mean Arterial Pressure • Constantly monitored by baroreceptors (pressure sensors) within circulatory system – Short-term control adjustments • Occur within seconds • Adjustments made by alterations in cardiac output and total peripheral resistance • Mediated by means of autonomic nervous system influences on heart, veins, and arterioles – Long-term control adjustments • Require minutes to days • Involve adjusting total blood volume by restoring normal salt and water balance through mechanisms that regulate urine output and thirst Fig. 10-11, p. 347 Carotid sinus baroreceptor Common carotid arteries (Blood to the brain) Neural signals to cardiovascular control center in medulla Aortic arch baroreceptor Aorta (Blood to rest of body) Fig. 10-35, p. 371 Parasympathetic stimulation Sympathetic stimulation Heart Heart rate Cardiac output Heart Contractile strength of heart Arterioles Veins Cardiac output Heart rate Vasoconstriction Vasoconstriction Venous return Blood pressure Blood pressure Stroke volume Total peripheral resistance Stroke volume Cardiac output Blood pressure Blood pressure Fig. 10-37, p. 372 Baroreceptor Reflexes to Restore Blood Pressure to Normal Normal Arterial pressure (mm Hg) Increased Decreased 120 80 Firing rate in afferent neuron arising from carotid sinus baroreceptor Time Fig. 10-36, p. 371 Blood Pressure • Additional reflexes and responses that influence blood pressure – Left atrial receptors and hypothalamic osmoreceptors affect long-term regulation of blood pressure by controlling plasma volume – Chemoreceptors in carotid and aortic arteries are sensitive to low O2 or high acid levels in blood – reflexly increase respiratory activity – Associated with certain behaviors and emotions mediated through cerebral-hypothalamic pathway – Exercise modifies cardiac responses – Hypothalamus controls skin arterioles for temperature regulation – Vasoactive substances released from endothelial cells play role Blood Pressure Abnormalities • Hypertension – Blood pressure above 140/90 mm Hg – Two broad classes • Primary hypertension • Secondary hypertension • Hypotension – Blood pressure below 100/60 mm Hg Hypertension • Most common of blood pressure abnormalities • Primary hypertension – Catchall category for blood pressure elevated by variety of unknown causes rather than by a single disease entity – Potential causes being investigated • • • • • • • • Defects in salt management by the kidneys Excessive salt intake Diets low in K+ and Ca2+ Plasma membrane abnormalities such as defective Na+-K+ pumps Variation in gene that encodes for angiotensinogen Endogenous digitalis-like substances Abnormalities in NO, endothelin, or other locally acting vasoactive chemicals Excess vasopressin Hypertension • Secondary hypertension – Accounts for about 10% of hypertension cases – Occurs secondary to another known primary problem – Examples of secondary hypertension • Renal hypertension • Endocrine hypertension • Neurogenic hypertension Hypertension • Complication of hypertension – Congestive heart failure – Stroke – Heart attack – Spontaneous hemorrhage – Renal failure – Retinal damage Hypotension • Low blood pressure • Occurs when – There is too little blood to fill the vessels – Heart is too weak to drive the blood • Orthostatic (postural) hypotension – Transient hypotensive condition resulting from insufficient compensatory responses to gravitational shifts in blood when person moves from horizontal to vertical position Hypotension • Circulatory shock – Occurs when blood pressure falls so low that adequate blood flow to the tissues can no longer be maintained – Four main types • • • • Hypovolemic (“low volume”) shock Cardiogenic (“heart produced”) shock Vasogenic (“vessel produced”) shock Neurogenic (“nerve produced”) shock Circulatory shock ( mean arterial pressure) Cardiac output Cardiac output Total peripheral resistance Widespread vasodilation Loss of blood volume Loss of fluids derived from plasma Severe hemorrhage Excessive vomiting, diarrhea, urinary losses, etc. Hypovolemic shock Weakened heart Cardiogenic shock Vasodilator substances released from bacteria Histamine released in severe allergic reaction Septic shock Anaphylactic shock Cardiogenic shock Loss of vascular tone Sympathetic nerve activity Neurogenic shock Fig. 10-39, p. 377 Fig. 10-40, p. 378