ACUTE PNEUMONIA IN CHILDREN
advertisement
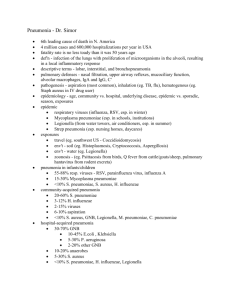
ACUTE PNEUMONIA IN CHILDREN Department of pediatrics ACUTE PNEUMONIA IN CHILDREN • Pneumonia is an inflammation of the parenchyma of the lung, • Incidence 0.026 episodes per child/year in USA, • 0.28 episodes per child/year in developed countries SYMPTOMS AND SIGNS • • • • • • • Raised respiratory rate - 50 per minute or more if child 2mo up to 12mo; - 40 per minute or more if child 12 mo up to 5 yr - 30 per minute or more if child above 5 yr Stridor in calm child or wheezing Fever >37.5o Dry cough or production of sputum Worse signs: the child is not able to drink or feeding wall, vomit everything, is lethargic or had convulsions Focal chest signs- chest indrawing - decreased expansion - dullness on percussion - bronchial breathing - pleural chest pain in older children ETIOLOGY • Viruses: influenza A and B, RS, adenovirus, parainfluenza • Gram + bacteria: Str.pneumoniae, Str.pyogenes, Staph.aureus • Gram- bacteria: H.influenzae, Kl.pneumoniae, Ps.aeruginosa, Morax. catarrhalis, Neis. meningitides, E.coli, Proteus, Enterobacter. • Atypical nonbacterial bacilli: Mycoplasma or Chlamydia pneumoniae,Legionella (acquired by breathing droplets or contaminated water) • Specific pneumonia in infants: aspiration (diminished gag reflex), gastroesophagal reflux, heart defects, genetic disorders, asthma, impaired immune system. CLINICAL MANIFESTATIONS • History- recent respiratory infection, exposure to people with pneumonia, fever, acute or persistent cough, dry/productive, related to feeding (aspiration), choking/ staccato/paroxysmal (foreign body aspiration, pertussis). • Worse signs: not able to drink or feeding, vomit everything, is lethargic or had convulsions • Physical examination-confusions, abnormally sleepy, cyanosis, fast breathing, nasal flaring, respiratory distress, grunting, stridor, wheezing; - vomiting, diarrhea, abdominal pain in paralytic ileus; - dullness on percussion: -consolidation or pleural effusion, empyema; - auscultation- rales, crackles, crepitations, rhonchi (rumblings). - clinical signs that predict death in children:worse signs, prolonged illness, severe X-ray changes, cyanosis, leukocytosis, hepatomegaly. PNEUMONIA- DIAGNOSIS • Chest X-ray confirms pneumonia and pleural effusion or empyema - Confluent lobar consolidation is typically in pneumococcal causes - Viral pneumonia- hyperinflation with bilateral interstitial infiltrates • Bronchoscopy, USG, CT scan in malformation or tumors • WBC in viral pneumonia are normal or <15,000/ml, with lymphocyte rises; in bacterial WBC>20,000/ml, granulocyte rises • Atypical pneumonia: a higher WBC, ESR and C-reactive protein • DNA, RNA, antibodies tests for the rapid detection of viruses • PCR test or seroconversion in an IgG assay • Serologic evidence of the ASL-O • Serum IgE in recurrent wheezing • Isolation of the bacteria from the blood, pleural fluid or lung • Culture of sputum and susceptibility of the antibiotics • Urinary antigen test positive PNEUMONIA -TREATMENT ANTIBIOTIS: 1.Penicillins and betalactams: Amoxycillin, Amoxi/Clav, Sulbactam 2.Cephalosporines- Cefazolin, Cefuroxim, Ceftriaxon, Ceftazidizime 3.Penems- Imipenem/Cilastatin, Meropenem, Ertapenem 4.Quinolones-Ciprofloxacin, Levofloxacin, Moxifloxacin, Gatifloxacin- more effective in Gram- bacteria 5.In atypical pneumonia – macrolides: Clarithromycin, Roxithromycin, Azithromycin (7.5-15mg/kg/day) 6.Aminoglycosides- dosage according to age, weight and kidney function (Gentamicin, Tobramycin, Amikacin) 7.In viral pneumonia treatment withhold antibiotics SUPPORTIVE TREATMENT 1. good hydration, cough remedies, antipyretics, oxygen in the central cyanosis or worse signs 2. For children with wheeze- rapid acting bronchodilator(Salbutamol) 3. Drainage with tube in empyema, fibrinolytic therapy: urokinase, streptokinase, alteplase 4. Indications for hospitalization: age <6mo, persistent fever, worse signs, severe respiratory distress, toxic appearance, no response to antibiotic RESPONSE TO TREATMENT • The factors then patients leads to “Slowly resolving pneumonia”: 1. complications such as empyema 2 .bacterial resistance 3.viral causes, foreign bodies or food aspiration 4. bronchial obstruction 5.pre-existing immunodeficiencies 6. cyliary dyskinesia, cystic fibrosis, other noninfectious causes. The first step- repeat chest X-ray COMPLICATIONS ● The result of direct spread in the thoracic cavity: pleural effusion, empyema, pneumothorax, pericarditis ● Hematologic spread:sepsis, meningitis, arthritis, osteomyelitis PREVENTION OF PNEUMONIA ● Immunization against H. influenzae type b ● Influenza vaccine ● Heptavalent pneumococcal conjugate vaccine ● Health education of the community ● Messages for mothers to recognize the signs of pneumonia REFERENCES 1.Nelson textbook of pediatrics, 18-th edition, 2007, p.1795-1800 2.Dr Herman Laferi-Community acquired pneumonia, diagnosis, treatment, Satellite Symposium “Update in Infectious Pathology”, 2006, Chisinau 3.Technical bases for WHO recommendations on the management of pneumonia in children at first-level health facilities, Geneva, 2001